Ankle fractures
(Broken ankle)
Ankle fractures, known more commonly as a “broken ankle,” happen when there is a break in one or more of the bones that make up the ankle joint. Although fractured ankles are an injury seen in almost every age, they are more prevalent in older and more active generations.
As bones break, the ankle becomes more unstable. A fractured ankle can become a severe issue when the ligaments are also damaged.
Luckily, there are both surgical and nonsurgical treatment options available. A physician should check all ankle fracture injuries to determine severity.
Anatomy
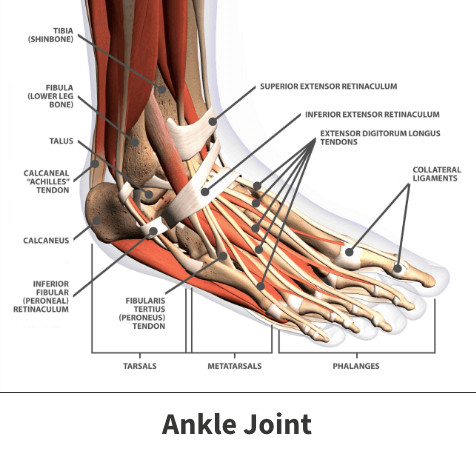
The ankle is a major ball-and-socket joint connecting three major leg bones. These are the three bones that make up the ankle joint:
- Tibia – Shinbone
- Talus – Bone that sits between the heel bone, tibia, and fibula
- Fibula – Lower leg bone
Ankle fractures are classified by the area of bone that is broken. The ankle is made up of parts of the tibia and fibula:
- Medial malleolus – Inside part of the tibia
- Posterior malleolus – Back part of the tibia
- Lateral malleolus – End of the fibula
Two joints are involved in fractures of the ankle:
- Ankle joint (tibia, talus, fibula)
- Syndesmosis joint (between the tibia and fibula, held together by ligaments)
The strength of the ligaments and bones determines the stability of the ankle.
About
Ankle fractures occur when one of these bones sustains some type of breakage.
Fractures occurring on the inside shinbone are called medial malleolus breaks. Those impacting the shinbone’s rear are known as posterior malleolus, while injuries to the lower leg bone’s end are classified as lateral malleolus fractures.
Fractures are also categorized by their severity. Nondisplaced fractures are those in which affected bones did not shift out of place. Displaced fractures involve the shifting of bone fragments. Open or compound fractures happen when wounded bone sustains significant abnormal shifts and might break through the skin or other structures like soft tissues and blood vessels.
Causes
Broken ankles typically result from sudden forceful or abnormal movements caused by falls from notable heights, impact from acute events like automobile accidents, and unusual twisting or rolling. Tripping, falling, rolling your ankle, or rotating it wrong can also create an ankle fracture. Depending on your age and health condition, this issue can become far more severe if left untreated.
Risk factors
Your risk of sustaining a broken ankle increases if you:
- Play contact sports like football or basketball.
- Play sports requiring quick and awkward twists and turns, such as gymnastics, tennis, and soccer.
- Increase your physical activity level too quickly.
- Use old or worn shoes when engaging in any type of exercise.
- Fail to properly stretch ankle joints and muscles before workouts or athletic competition.
- Live in a very messy or cluttered environment.
An individual’s risk can also increase if they have medical conditions leading to bone weakening like osteoporosis or smoke cigarettes, which may increase their risk of developing osteoporosis and cause bone-weakening events like inflammation.
Fractured ankle symptoms
Since a sprain can sometimes feel the same as a broken ankle, it is always important to consult your physician. Evaluating the symptoms of an ankle fracture can determine if that is the issue at hand.
Common symptoms of an ankle fracture include:
- Immediate pain
- Severe pain
- Bruising
- Swelling
- Tenderness
- Cannot put weight on the injured foot
- An “out of place” deformity (especially if the ankle joint is dislocated)

Diagnosis
Your Florida Orthopaedic Institute physician will discuss your medical history and symptoms with you. They will also ask about how the injury occurred and examine the affected area.
If your physician believes you may have fractured your ankle, they will order imaging tests to examine the injury more fully. These could be:
- X-rays – X-rays can show if the ankle bone has been broken and how many pieces of broken bone there are. They can also determine if displacement (the gap between broken bones) exists. Your physician may also choose to take X-rays of other portions of the leg or foot to ensure that nothing else was damaged in the injury.
- Stress test – A stress test is done to determine if surgical procedures are necessary to assist the injury in healing. Your physician will put pressure on the ankle and take a special x-ray to determine such.
- CT scan (Computed Tomography) – If the fracture extends into the ankle joint, a CT scan may be needed to investigate the injury further. CT scans create a cross-section image that your physician can check to see the injury’s severity.
- MRI scan (Magnetic Resonance Imaging) – If your physician suspects ligament damage has occurred, they may order an MRI scan to get a closer look. MRI scans can look deeper into bones and soft tissues, such as ligaments, to create higher-resolution images than most other tests.
Treatment for ankle fractures
Doctors consider several factors before treating an ankle fracture, such as the patient’s age, general health, physical fitness level, and weight, in addition to the fracture’s location and severity.
Simple, uncomplicated breaks may heal without the need for surgery. But nondisplaced fractures can result in significant ankle instability requiring corrective surgeries, and moderate to severe fractures typically need surgery to either repair or reposition the displaced bones.
If your physician determines that your ankle is fractured, they will determine the type of fracture injury and how to treat it.
- Lateral malleolus fracture
- Medial malleolus fracture
- Posterior Malleolus fracture
- Bimalleolar fractures/bimalleolar equivalent fracture
- Trimalleolar fracture
- Syndesmotic injury
Nonsurgical treatment
Ankle fractures can be healed via nonsurgical methods if the injury is not too severe or unstable.
- Lateral malleolus fracture (fracture of the fibula) – There are various fracture levels that may use multiple treatments. If your ankle is stable, there are nonsurgical treatment options available. These can range from wearing high-top tennis shoes to short-leg casts. Your physician may recommend waiting to put weight on the foot to ensure no fragments have moved out of place during healing.
- Medial malleolus fracture (break in the tibia at the inside of the lower leg) – If not out of place or very minor, this fracture can be healed after not putting stress on it for six weeks. A short leg cast or removable brace, along with the advice of your physician, will generally help the healing process move quicker.
- Posterior malleolus fracture (fracture of the back of the tibia at the ankle joint level) – In most cases, the fibula is also broken due to it sharing ligament attachments with the posterior malleolus. If the ankle is still stable, it can be treated without surgery. Treatment may be with a short leg cast or a removable brace. It is important to determine the severity so that arthritis does not develop.
- Bimalleolar fractures/bimalleolar equivalent fracture (two of the three parts of the ankle are broken) – A bimalleolar equivalent fracture indicates that ligaments on the inside of the ankle are also injured. Since these injuries are generally unstable, surgery is usually recommended. A splint and short leg cast can be applied in case health issues prevent surgery. You will need to see your physician regularly to ensure your ankle remains stable.
- Trimalleolar fracture (all three parts of the ankle are broken) – Since this is highly unstable, surgery is almost always recommended. The rare nonsurgical treatment options include a short leg cast, a splint, and consistent visits to your physician.
- Syndesmotic injury (the joint between the tibia and fibula that injures the ligaments and creates a fracture) – If the ligament is the only part injured, it can heal like an ankle sprain and can be treated by removing weight without surgery. Most cases include a ligament sprain and one or more fractures. These are highly unstable and do poorly without surgical treatment.
Surgical treatment
In the case that nonsurgical treatment options do not work, or your ankle is too unstable, your physician may recommend surgery.
- Lateral malleolus fracture – If the fracture is out of place, the bone fragments must be repositioned via surgery. Fragments would be placed back into their normal alignment and held together with special screws and metal plates attached to the outside surface of the bone.
- Medial malleolus fracture – Surgery may be recommended if the fracture is out of place, or in some rare cases even if it isn’t. Since the risk of the fracture not healing correctly is high, surgery may include bone grafting so that new bone can grow with the addition of screws and a metal plate. This can lower the risk of arthritis and allow movement to return quicker.
- Posterior malleolus fracture – Surgery may be recommended if the ankle is unstable. Screws can be placed from the front of the ankle to the back of the ankle or placed along the back of the shin bone in addition to a metal plate.
- Bimalleolar fractures/bimalleolar equivalent fracture – Surgery is suggested since the ankle is unstable with this type of fracture. These are treated with the same procedures listed above.
- Trimalleolar fracture – Since these fractures are incredibly unstable, surgery is highly recommended. These are treated with the same procedures listed above.
- Syndesmotic injury – These fractures are highly unstable and do poorly without surgical treatment. These are treated with the same procedures listed above.
Recovery
Every patient’s case is different, and fractures often heal at their own rate. Other factors determining such timeframes include one’s:
- Age
- Overall health
- Fitness level
- Injury history
- Lifestyle habits
Above all, the specific bone involved, and the fracture’s extent will often be key in determining the length of recovery. As a rule, uncomplicated nondisplaced injuries should heal faster than displaced wounds requiring surgery.
Prevention
Unexpected events like falls or car accidents are not always preventable. You can lower your chances of experiencing a broken ankle by:
- Maintaining a neat, tidy living space
- Stretching before participating in exercise or athletic competition
- Wearing new and comfortably fitting shoes
- Engaging in exercises designed to strengthen ankle and leg muscles
- Consuming a diet containing bone-strengthening nutrients like calcium and Vitamin D
- Gradually increasing the intensity of one’s workout
Those experiencing symptoms of an ankle fracture or injury should be evaluated by their doctor as soon as possible. Routine medical checkups might identify underlying injuries or illnesses capable of increasing their risk of experiencing a broken ankle.
Learn everything you need to know about ankle fractures, including information about types of fractures, treatment options, and more.
Videos
Related specialties
- Achilles Calcific Tendinitis
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fusion Surgery
- Arthroscopic Articular Cartilage Repair
- Arthroscopy of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Neuromas (Foot)
- Plantar Fasciitis
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
