Osteoarthritis of the hip
Osteoarthritis of the hip is a “wear-and-tear” disease. The cartilage of the hip joint gradually wears away over time, causing pain and stiffness. It can make it hard to do everyday activities like bending over to tie a shoe, rising from a chair, or taking a short walk.
Since osteoarthritis gradually worsens over time, the sooner you start treatment, the more likely it is that you can lessen its impact on your life. Unfortunately, there is no cure for osteoarthritis. But there are many nonsurgical and surgical treatment options available to help you manage pain, stay active, and live the best life you can.
Anatomy
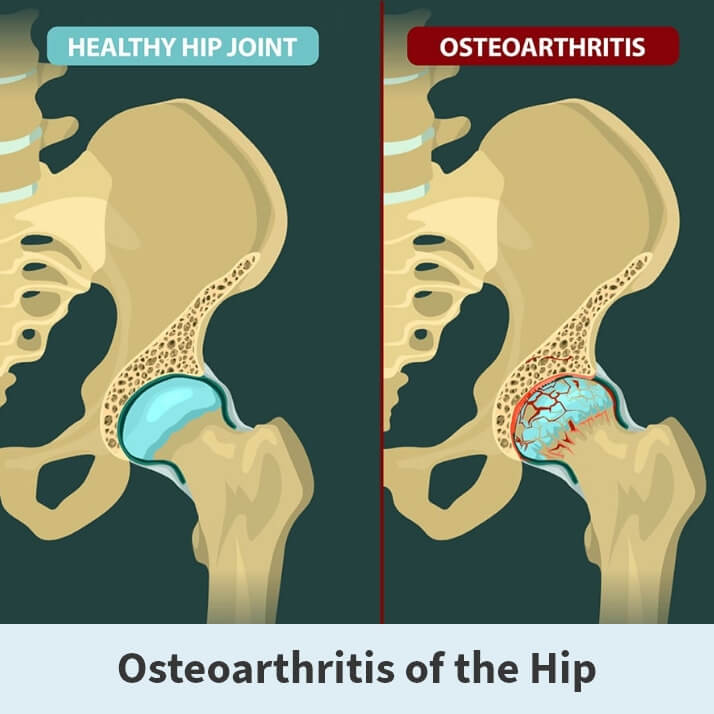
The hip is a ball and socket joint. The socket is formed by the large pelvic bone (acetabulum), and the ball is formed by the upper end of the thighbone (femoral head). A slippery tissue known as the articular cartilage covers the surface of the joint, creating a smooth surface that allows the bones to glide easily across each other. The large pelvic bone is ringed by strong fibrocartilage known as the labrum, which form a lining around the socket.
Also, the whole joint is surrounded by bands of tissue (ligaments) that form a capsule that acts to hold the joint together. The undersurface of the capsule is lined by a thin membrane (synovium), which produces synovial fluid to lubricate the hip joint.
About
Osteoarthritis of the hip is a degenerative type of arthritis that occurs most often in middle-aged people and older. This disease causes the cartilage in the hip joint to wear away gradually over time. As the cartilage wears away, it becomes frayed and rough, causing the protective space between the bones in the joint to shrink. As the space in the joint shrinks, the bones begin to rub against each other, resulting in pain and other unpleasant symptoms.
Additionally, to make up for the lost cartilage, the damaged bones may start to grow outward and form bone spurs (known as osteophytes).
There is no single specific cause of osteoarthritis of the hip. Still, several factors may increase your likelihood of developing the disease, including:
- Age
- Obesity
- Family history of osteoarthritis
- Improper formation of the hip joint at birth
- Previous injury to the hip joint
Symptoms
There are several symptoms associated with osteoarthritis of the hip.
Symptoms include:
- Pain around the hip joint that either worsens slowly over time or appears instantly
- Pain in your groin or thigh that radiates to your buttocks or your knee
- Pain that flares up with vigorous activity
- Stiffness in the hip joint that makes walking or moving difficult
- “Locking” or “sticking” of the joint or a grinding noise when you move caused by loose fragments of cartilage and other tissue interfering with the smooth motion of the hip
- Decreased range of motion that affects the ability to walk and may cause a limp
- Increased joint pain with rainy weather

Diagnosis
Your Florida Orthopaedic Institute physician will talk with you about your symptoms, medical history, and overall health, followed by a physical examination and imaging tests.
During the physical examination, your physician will look for:
- Pain when pressure is placed on the hip
- Any problems with the way you walk (your gait)
- Signs of injury to the muscles, tendons, and ligaments surrounding the hip
- Tenderness in and around the hip
- Decreased range of hip motion
- A grating sensation inside the joint during movement
The initial imaging test your physician will order is an X-ray. X-rays create detailed pictures of dense structures, such as bones. This test will show if your hip joint space has narrowed and any other changes in the bone. It can also indicate the formation of any bone spurs. Occasionally, a magnetic resonance imaging (MRI) scan, a computed tomography (CT) scan, or a bone scan may be needed to better determine the condition of the bone and soft tissues of your hip. These tests are not typically ordered but are available.
Treatment
There are many different nonsurgical treatments your physician may recommend, including:
- Lifestyle modifications – There are some changes you can make to your daily routine to help protect your hip joint and slow the progress of osteoarthritis. For example, you can minimize activities that aggravate the condition. These can include climbing stairs or switching from high impact activities like jogging or tennis to lower impact activities like swimming or cycling.
- Physical therapy – Specific exercises can help increase your range of motion and flexibility while also strengthening the muscles in your leg and hip. During physical therapy, you will perform individualized exercises that meet your needs and lifestyle.
- Assistive devices – Using walking supports like a crutch, cane, or walker can improve mobility and independence. Using assistive aids like a long-handled reacher to pick up low-lying things will help you avoid movements that may cause pain.
- Medications – If your pain affects your daily routine, your Florida Orthopaedic Institute physician may add one of the following medications to your treatment plan: Nonsteroidal anti-inflammatory drugs like Aleve (naproxen) and Advil (ibuprofen), cortisone (anti-inflammatory steroid) or Tylenol (acetaminophen, an over-the-counter pain reliever).
Surgical treatment
If nonsurgical treatment is ineffective or if your pain and symptoms are severe, your physician may recommend a surgical procedure. There are several different surgical treatments your physician may choose for you, such as:
- Osteotomy – A procedure that takes the pressure off the hip joint by cutting and realigning the head of the thighbone or the socket.
- Hip resurfacing – The damaged bone and cartilage in the hip socket (acetabulum) are removed and replaced with the metal shell. Then the head of the femur is capped with a smooth metal covering.
- Total hip replacement – During this procedure, both the damaged acetabulum and femoral head are removed and replaced by either a new metal, plastic, or ceramic joint.
Regardless of which surgical procedure is chosen, it takes some time to recover. During your recovery period, you will need physical therapy to regain strength and restore your range of motion. After your procedure, you may need to use a cane, crutches, or a walker for a short time. In most cases, surgery relieves the pain of osteoarthritis and makes it possible to perform daily activities more easily.
Videos
Related specialties
- Avascular Necrosis (Osteonecrosis)
- Groin Strains & Pulls
- Hamstring Injuries
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers & Trochanteric Bursitis
- Iliopsoas Tenotomy
- Labral Tears of the Hip (Acetabular Labrum Tears)
- Osteoporosis
- Pelvic Ring Fractures
- Piriformis Syndrome
- Sports Hernias (Athletic Pubalgia)
- Thigh Fractures
- Thigh Muscle Strains
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
