Is my swollen knee a reason to see a physician?

A swollen knee is a symptom of an injury, infection, overuse or chronic condition. But which one? All of the usual knee suspects, such as ACL injuries, arthritis and meniscus tears, might be the cause of your knee swelling and pain. To find out what’s really happening in your knee when it’s swollen, you need to dig deeper.
Swelling is a sign of knee fluid buildup. The medical term is knee joint effusion (meaning “water on the knee”). It can be a severe issue if your pain and stiffness are intense enough to make it hard to get around. Regardless of the severity, finding and treating the source of a swollen knee joint is crucial so it doesn’t worsen. In many cases, an experienced physician can diagnose the source of the swelling with just a history and physical exam. An X-ray or MRI can be helpful but isn’t always needed.
Read on to learn what causes knee swelling, the best knee swelling treatments, and when it’s severe enough to see a specialist.
Why is there swelling in my knee?
There are dozens of reasons why you might have a swollen knee. These potential reasons may be classified as traumatic or non-traumatic.
Traumatic causes are those that involve a significant knee injury, such as twisting your knee (while landing from a jump) or a direct hit to the knee. In either case, there is an acute change in knee function at the time of injury. Non-traumatic causes are considered passive (they develop because of overuse, wear and tear or chronic degenerative diseases).
Both are common among athletes and the general population alike.
Events associated with traumatic swelling in knees
Swelling that is considered traumatic is caused by hard blows to the knee. It is also linked to jarring or twisting movements. The most common traumatic incidents associated with knee swelling include car accidents, bad falls and sports injuries.
Typically, there is immediate knee pain followed by swelling and decreased function, such as the ability to bend or bear weight on the injured knee. It may indicate a serious injury to the knee joint, bone or surrounding soft tissue.
Bone injuries that can cause a swollen knee
Swelling is a symptom of two common types of knee bone injuries:
- Dislocations: Two main types of knee dislocations cause swelling:
- Kneecap dislocation (patella dislocation) is a common injury in adolescents and young adults.
- Knee dislocation is a medical emergency that results from a high-energy injury that causes the thigh bone (femur) and shin bone (tibia) to no longer be aligned. These occur with multiple ligament tears and are usually associated with other damage in the joint (meniscus, articular cartilage). There may also be an additional injury, including fractures and damage to the surrounding nerves and blood vessels.
- Fractures: A break in one of the three knee bones—the thigh bone (femur), shin bone (tibia) or kneecap (patella)—is called a fracture.
Traumatic knee swelling
Collateral Ligament Tears
The knee has four main ligaments- anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL) and lateral collateral ligament (LCL). Sprained ligaments are often associated with symptoms of knee pain and swelling.
The knee’s collateral ligaments control side-to-side stability and protect the joint against sudden movements. The medial collateral ligament (MCL) is on the inside part of the knee and connects the femur to the tibia. In contrast, the lateral collateral ligament (LCL) is on the outside part of the knee and also connects the femur to the tibia.
Injury is caused by a direct impact to the opposite side of the knee (for example, the MCL is injured by forceful contact to the outside of the knee, which forces the knee inward, resulting in stretching or tearing the MCL. MCL injuries are much more common than LCL injuries.
Most MCL sprains heal without surgery and require bracing and physical therapy before returning to sports. LCL injuries, if associated with other ligament tears, often require surgery to repair and reconstruct all damaged structures.
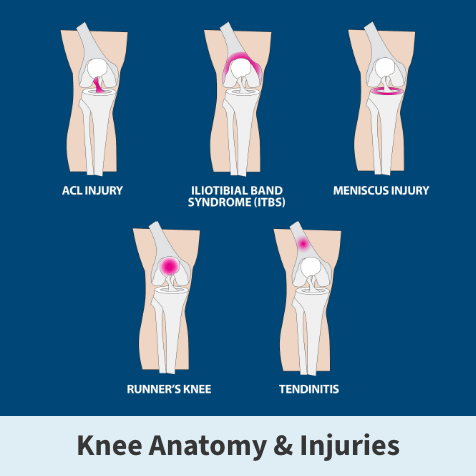
Anterior cruciate ligament (ACL) tears
This ligament runs diagonally in the middle of the knee and helps keep the shin bone (tibia) from sliding forward in the thigh bone (femur). It also provides rotational stability by preventing the shin bone (tibia) from rotating on the thigh bone (femur). Tears usually present with ACL injury symptoms that include moderate to severe swelling and the knee feeling unstable.
ACL tears can result from contact (e.g., direct blow to the knee) or non-contact injuries (e.g., hyperextension, deceleration, twisting/pivoting). Most ACL tears are from non-contact injuries. Complete ACL tears usually require surgery for athletes to return safely to their sport.
Posterior cruciate ligament (PCL) tears
The posterior cruciate ligament mirrors the ACL, running diagonally but in the opposite direction of the ACL. The result is a crossing of the two ligaments, forming an “X” in the middle of the knee.
The primary function of the PCL is to keep the shin bone (tibia) from sliding backward in relation to the thigh bone (femur). Patients with PCL injuries usually present with complaints of swelling and pain in the back of the knee and rarely complain of instability. Most isolated PCL tears do not require surgery and improve with bracing and physical therapy.
Meniscus tears
The meniscus is a type of specialized cartilage found in the knee.
Each knee has a meniscus on the inside (medial meniscus) and outside (lateral meniscus) part. It is horseshoe-shaped and sits between the shin bone and the thigh bone. The meniscus has many functions but primarily acts as a shock absorber of the knee. This protects the articular cartilage by helping to dissipate load across the joint with weight-bearing activities like walking and running.
Non-contact twisting and pivoting injuries and direct blows during sports can damage a meniscus. The meniscus also weakens as we age, and older patients may develop meniscus tears with no history of any injury or trauma.
One symptom distinguishing a meniscus tear from other injuries is the feeling of the knee “locking up” and being unable to straighten fully.
Articular cartilage injuries
Articular cartilage is a layer of specialized cartilage that covers the bony ends of nearly all joints in the body, including the knee. This provides a perfectly smooth surface so your joints move without friction and with no pain. Arthritis occurs when the articular cartilage wears away, and if severe enough, may result in the need for a knee replacement.
Articular cartilage can also be damaged and torn during a fall, collision, or aggressive twisting and pivoting, as seen in sports. Articular cartilage tears are more common in the knee than in other joints and may be associated with other ligament or meniscus damage.
Articular cartilage injuries typically present with pain and significant swelling (knee effusion). An MRI scan helps make the correct diagnosis. Depending on the size, location, and degree of cartilage damage, articular cartilage injuries often require advanced regeneration or replacement surgery.
Patella Dislocations
A patella (knee cap) dislocation occurs when the kneecap is out of alignment. Like an ACL sprain, this may occur with or without a contact injury. It’s most common among kids and young adults who play sports. It’s possible to pop the kneecap back in place if it’s not too painful, but if you do, see a knee specialist afterward to check for a fracture or other associated problems.
Patients often hear an audible ”pop” at the time of injury, followed by intense pain, buckling, sudden swelling, visible dislocation with deformity, and inability to move or straighten the knee.
Treatment involves manually putting the kneecap back in place, recovery at home (rest, ice, compression, elevation, over-the-counter meds), physical therapy, bracing, and an MRI to check for further damage. Surgery may be necessary if there are other significant injuries to the knee or if the patient has recurrent episodes of patella instability where the kneecap dislocates.
Tendon tears
The patellar tendon connects the bottom of the kneecap (patella) to the shinbone (tibia). A tear or rupture can mirror ACL injury symptoms and occur during the same activities. However, a torn patellar tendon might create an indentation below the kneecap, and the patella will be higher up the leg since it’s no longer attached to the bone below it.
The quadriceps tendon connects the thigh muscle to the top of the kneecap. When it tears, an indentation will appear above the kneecap where the tendon tears off the top of the patella. The kneecap will also be lower than usual since the tendon no longer pulls it up to its usual position.
Both of these injuries result in acute pain, severe swelling, inability to actively straighten the knee, and difficulty walking. Surgery is required to reattach the torn tendon to the kneecap.
Bone Bruises
A bone bruise or microfracture can occur from a contact or non-contact injury. Contact injuries include such things as a motor vehicle accident where the knee hits the dashboard or sports like football where a player takes a helmet to the knee. Non-contact injuries from twisting, pivoting, or hyperextending the knee may also cause a bone bruise.
These microfractures aren’t severe enough to appear on X-rays and require an MRI for diagnosis. They cause bleeding of the involved bone into the joint with significant swelling. Unless there are other associated injuries, bone contusions will heal with conservative treatment and do not require surgery.
Non-traumatic knee swelling
You might wonder, “If I didn’t have an accident, why is my knee swollen?” In this case, your swollen knee must have a non-traumatic cause (these are causes that don’t involve a specific injury and may occur gradually).
Arthritis
Two main types of arthritis are osteoarthritis (wear and tear arthritis) and Inflammatory arthritis (rheumatoid arthritis, gout, lupus, etc.)
Bursitis
Knee swelling is a common symptom of bursitis, which—in this instance—involves inflammation of the bursae (or fluid-filled sac that is located just under the skin in front of the knee cap). Bursitis can occur from overuse or direct trauma. It is essential to distinguish between swelling from bursitis (superficial fluid in the bursa sac outside the knee joint) from a true joint effusion (swelling within the knee joint itself).
Infection
The knee joint can become infected through an open wound (germs entering the joint) or by the bloodstream due to an infection elsewhere in the body. This can result in severe knee pain, swelling, redness, and difficulty walking. The knee will feel warm to the touch. Patients often feel “sick” and may have a high fever. Treatment usually includes IV antibiotics and an arthroscopic “wash out” of the joint.
When to see a physician for care of a swollen knee

If you’re experiencing any of these symptoms in addition to knee swelling, you should see a specialist as soon as possible if you:
- Have a fever,
- Are vomiting,
- Notice the area around your injured knee is warm and tender,
- Can’t bear weight on the affected leg,
- Notice your knee feels unstable and
- Can’t bend or straighten your knee
Many underlying causes of knee joint swelling can be treated at home with rest, ice, elevation and over-the-counter anti-inflammatory medication. After a few days, if the swelling worsens or the pain interferes with your normal activities, see a physician.
Treatments for swollen knee
Treatment may vary depending on the underlying cause, severity, age and lifestyle of the patient. Options include:
- Physical therapy,
- Bracing or splinting,
- Injections (steroid, viscosupplementation (gel), PRP) and
- Surgery.
FAQs about swollen knees
Ice or heat? Rest or exercise? Here’s advice on how to handle knee swelling.
Is heat or ice better for treating swelling of the knee?
Ice is the most common remedy for a swollen knee]. Use it for the first 24-48 hours after an injury. Then, you may continue to use ice to reduce knee swelling or alternate with heat if you have chronic stiffness.
How do I know if my knee swelling is serious?
If the pain and swelling in your knee don’t respond to conservative at-home treatment (rest, ice, compression, elevation and over-the-counter medication), it is time to see a knee specialist.
Other signs that swelling isn’t ordinary include severe pain, knee deformity, inability to straighten or bend the knee, difficulty walking, redness, numbing or tingling below the knee, fever and nausea.
What increases the risk of developing a swollen knee?
Age, being overweight, poor physical condition and playing sports increase the risk of experiencing knee joint swelling or inflammation.
Age and poor physician condition cause weakness, which makes the knee more susceptible to injury. Excess weight puts the knee under strain and can cause inflammation. Explosive pivoting and twisting movements are common causes of sports knee injuries. Starting a new exercise program and progressing too rapidly is a common mistake that may lead to knee pain and swelling.
Other risk factors include poor balance (which can lead to falls) and routinely skipping athletic preparation and recovery.
Will drinking water help with knee swelling?
Proper hydration is essential for optimal athletic performance. However, drinking water will not help reduce joint swelling once a knee is swollen.
What is the best over-the-counter medicine for knee swelling?
For inflammation, nonsteroidal anti-inflammatory drugs (NSAIDs)—like Advil or Aleve—can help reduce inflammation and alleviate pain. These drugs work best in concert with icing (20 minutes at a time) frequently throughout the day.
What is the best sleeping position if I have some swelling in the knee?
Sleeping on your back with a pillow under the swollen knee is usually the most comfortable position. Elevating the knee above the heart can also help reduce inflammation. Avoid painful activities, and use crutches if you are limping.
Is it better to keep up with exercise or rest if my knee is swollen?
Let your knee rest for at least 48 hours if you notice swelling. Most people can gradually resume activities after a few days of rest if their knee swelling and pain resolve. Generally, it’s always best to exercise only if you can do so safely. While exercise can help you overcome a swollen knee by increasing its strength and flexibility, you should see a physician if your swelling returns or you experience any pain.
Get the world-class care for your knees at FOI
You don’t need to have experienced a serious injury to seek medical attention for a swollen knee. If you suspect your swelling is out of the ordinary, Florida Orthopaedic Institute’s experts can help.
FOI’s compassionate healthcare providers utilize a multidisciplinary approach and employ innovative, state-of-the-art treatments for all patients. Our specialists include orthopedic sports medicine surgeons, primary care sports medicine doctors, physical medicine and rehabilitation specialists, nurse practitioners, physician assistants, chiropractors, podiatrists, physical therapists, and certified athletic trainers.
Our orthopedic urgent care centers ensure timely and convenient initial evaluation and treatment access while facilitating prompt referral to the appropriate specialist. Additionally, we offer advanced imaging, including X-rays, ultrasound, CT and MRI scans. Our highly skilled physical therapists provide advanced rehabilitation techniques to maximize recovery. Trained specialists staff a durable medical equipment department to properly fit all casts, braces, crutches, etc. Patients receive the entirety of their care at one of our convenient locations throughout the Tampa Bay area.
Sitting out from the sport you love can be just as painful as an injury. The sports medicine specialists at Florida Orthopedic Institute are passionate about helping you return to action safely and as soon as possible.
Schedule with a physician or request an appointment to begin your recovery with FOI.
You might also like:
- Which Sports Knee Injury Do I Have?
- When are ACL Injury Symptoms Serious Enough to See a Physician?
- Pain Behind Knee & Calf—Here’s What It Could Mean
- Stepping Back Onto the Soccer Field After an ACL Injury
- Pickleball for Seniors: 10 Tips for Pain-Free Play
Our 10 most asked sports medicine questions
January 3, 2025