Anatomy
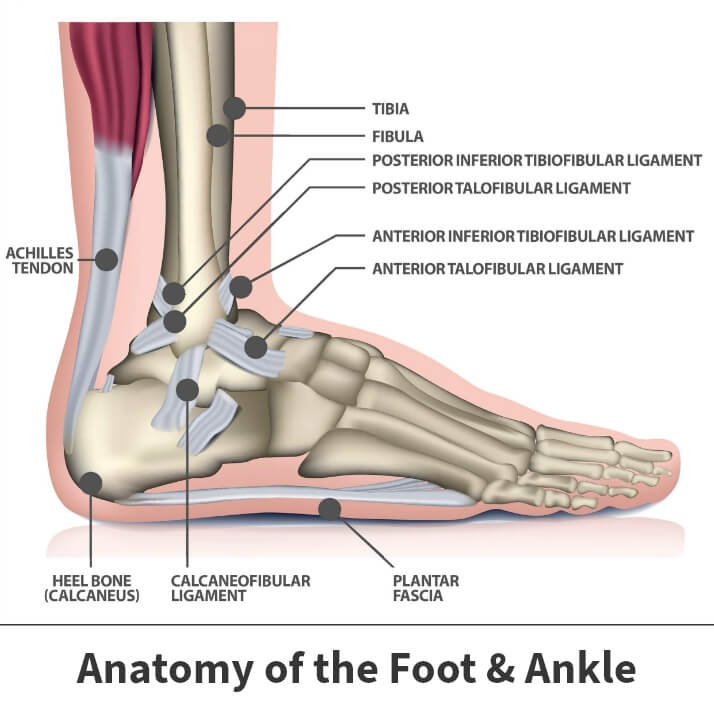
Connecting the heel to the front of the foot to support the arch, the plantar fascia is a thin and long ligament. Lying beneath the skin on the bottom of the foot, it is very fibrous.
About
Whether moving around normally day-to-day or in rapid physical activity, the plantar fascia absorbs the high stresses from such activity. Since too much stress can overwhelm the plantar fascia, the body responds with the plantar fascia becoming inflamed. This results in heel pain and stiffness, and in extreme cases, the tissues can be damaged or torn.
There is generally no reason for plantar fasciitis developing, although there are factors that can make you more susceptible to it:
- Obesity
- New or increased activity
- Tighter calf muscles
- Very high arches
- Repetitive impact activity
Unfortunately, heel spurs can occur in those who have plantar fasciitis. Heel spurs occur in 1 out of 10 people, with only 1 out of 20 people (or 5%) having foot pain. Despite heel spurs being linked to plantar fasciitis, they are not the cause of it. Luckily, the pain from plantar fasciitis can be treated without removing the spur.
Symptoms
The symptoms of plantar fasciitis range from mild to intense, generally including:
- Greater pain after (not during) exercise/activity
- Pain after getting out of bed in the morning or a long period of rest (starting with the first few steps and lessening after walking for several minutes)
- Pain on the bottom of the foot near the heel
Facts about plantar fasciitis
- Heel spurs do not cause plantar fasciitis
- Active men between 40-70 are most affected
- Improper footwear (not enough arch support), running on uneven surfaces, long distance running and downhill running are contributing factors
- Arch problems in the foot (flat feet or high arches) are factors
- Sudden weight gain or obesity can be a cause

Diagnosis
Your Florida Orthopaedic Institute physician will examine your foot and listen to your symptoms. They will also ask about your physical activity history.
Once your physician begins examining your foot, they will look for:
- Limited upward mobility of the ankle
- An area in front of your heel bone where the greatest tenderness occurs (on the bottom of your foot)
- A high arch
- Pain that worsens when you flex your foot
After the examination, your physician may order imaging tests to ensure that plantar fasciitis is causing the heel pain and not another issue.
X-rays can provide clear bone images and allow for your physician to see if arthritis or fractures come into play. Heel spurs can also be seen on x-rays.
Other imaging tests such as magnetic resonance imaging (MRI) and ultrasound might be ordered in the rare case that pain is not altered by treatment.
Treatment
Luckily, more than 90% of patients with plantar fasciitis will show improvement within a few months of treatment, which can greatly improve mobility.
Nonsurgical treatment
In most cases, plantar fasciitis can be treated at home. These simple treatments can include:
- Rest – Although difficult, decreasing or stopping the activities that are causing you the heel pain will help reduce it.
- Stretching – Performing stretches such as calf stretches and plantar fascia stretches can allow for a better range of motion in the foot along with improved stability.
- Nonsteroidal anti-inflammatory medication – Drugs such as naproxen (Aleve) or ibuprofen (Motrin) reduce pain and inflammation.
- Ice – Rolling your foot over a bottle full of cold water or ice for 20 minutes each day can be effective in alleviating pain.
- Night splints – A night splint allows for the plantar fascia to be stretched while sleeping.
- Physical therapy – In the case that at-home exercises aren’t working, your physician may recommend seeing a physical therapist to continue to assist in rebuilding strength.
- Cortisone injections – Cortisone, a powerful steroid, may be injected into the plantar fascia to reduce pain.
- Supportive shoes and orthotics – Thick-soled shoes with extra cushioning can reduce pain with standing and walking.
Surgical treatments
In the most extreme cases, surgery may be recommended. This typically only occurs after months of simple nonsurgical treatment. Some surgical treatments may include:
- Gastrocnemius recession – A surgical lengthening of the calf. Generally due to calf muscle tightness, one or two of the muscles are lengthened to increase mobility. This can be performed with a small incision and an endoscope, which contains a small camera.
- Plantar fascia release – If your range of motion is unaffected, but you are still experiencing pain, your physician may recommend that the plantar fascia ligament is partially cut to relieve tension in the tissue.
Related specialties
- Achilles Calcific Tendinitis
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Arthroscopic Articular Cartilage Repair
- Arthroscopy of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Neuromas (Foot)
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
