Rheumatoid arthritis of the hand
Rheumatoid arthritis of the hand is a disease that results in the swelling of the joint lining. The disease invades the surrounding tissues and produces a chemical that destroys the joint surface. The main symptoms are deformities in the hand and pain that gets worse over time and may require arthritis surgery.
Depending on the severity of your rheumatoid arthritis, either a nonsurgical or surgical treatment plan is recommended for arthritis surgery. If your rheumatoid arthritis is not severe, then your physician will recommend nonsurgical treatments. Unfortunately, neither treatment type can reverse any damage done to the joint. Both of these treatments help reduce symptoms and help you return to your daily routine.
Anatomy
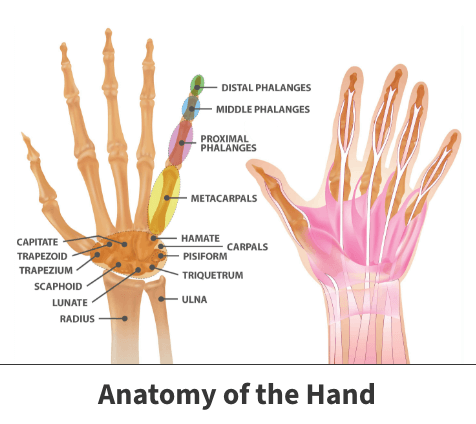
The bones in your hand include:
- Phalanges – These are the small bones that form the thumb and fingers. There are two phalanges in the thumb and three in each of the fingers.
- Metacarpals – These are the five bones located in the palm
Between these bones are joints which allow you to move your fingers.
About
Rheumatoid arthritis of the hand is a disease in which the joint lining in your hand swells, invades surrounding tissues, and produces chemical substances that attack and destroy the joint surface. The disease usually begins in middle age. Without proper treatment, rheumatoid arthritis can become a chronic, disabling condition.
Researchers believe that some people have genes that make them susceptible to the disease. People with these genes do not automatically develop rheumatoid arthritis. There is usually a trigger such as an infection or environmental factor that activates the rheumatoid arthritis gene. When the body is exposed to this trigger, the immune system responds inappropriately, resulting in rheumatoid arthritis.
If you have rheumatoid arthritis, your ligaments and joint capsules become less effective supporting structures. Erosion of the articular cartilage, together with ligamentous changes, results in deformity and contractures in the hand. As the disease progresses, pain and deformity increase.
Symptoms
There are several symptoms associated with rheumatoid arthritis.
These symptoms include:
- Swelling, pain, and stiffness in the joints in the hand
- A warm feeling around the joint
- Deformities and contractures of the joint
- Weakness due to anemia caused by low red blood cell count
- Nodules, or lumps, particularly around the elbow
- Fever
- Cysts
- Loss of appetite
- Decreased energy

Diagnosis
Your Florida Orthopaedic Institute physician will take a look at your symptoms and overall health and medical history.
A blood test may reveal an antibody called rheumatoid factor, an indicator of rheumatoid arthritis. X-rays can help show the progression of the disease.
The American College of Rheumatology requires at least four of the following seven criteria to confirm the diagnosis:
- Arthritis of hand joints for at least six weeks
- Arthritis on both sides of the body for at least six weeks
- Rheumatoid nodules under the skin
- Rheumatoid factor in blood testing
- Morning stiffness around the joint that lasts at least one hour
- Arthritis of three or more joints for at least six weeks
- Evidence of rheumatoid arthritis on X-rays
Treatment
Your treatment plan will be tailored for you as rheumatoid arthritis of the hand varies greatly depending on the severity. It is important to seek help early so that treatment can begin for arthritis surgery
Nonsurgical treatments
Nonsurgical treatments options include medication, injections, and splinting. The following factors are used to determine if nonsurgical treatments are the right option:
- How far your arthritis has progressed
- The number of joints involved
- Your age, activity level, and other medical conditions
- Ability to follow a treatment program
Medications are used to treat symptoms but unfortunately cannot restore joint cartilage or reverse any joint damage. The most common medications for arthritis are anti-inflammatories, which stop the body from producing chemicals that cause joint swelling and pain. Examples of anti-inflammatory drugs include medications such as Aleve (naproxen) and Advil and Motrin (ibuprofen).
Injections may also be used to treat your rheumatoid arthritis of the hand. These typically contain a long-lasting anesthetic and a steroid that can relieve pain for weeks to months. These injections can be repeated a limited number of times, due to possible side effects, such as lightening of the skin, weakening of the tendons and ligaments and infection.
Many cases can be managed with a class of medications called anti-rheumatic drugs. These medications slow the progression of joint damage. They are called disease-modifying antirheumatic drugs (DMARDs) and can play an important part of an overall treatment plan. Your rheumatologist will prescribe these types of medications.
Disease-modifying drugs act on the immune system to slow the progression of rheumatoid arthritis. This is why they are called “disease-modifying.” Many different drugs can be used as DMARDs in the treatment of RA, but some are used more often than others.
- Hydroxychloroquine (Plaquenil)
- Sulfasalazine (Azulfidine)
- Leflunomide (Arava)
- Methotrexate (Otrexup, Xatmep, Trexall, and Rasuvo) – the most commonly used DMARD
- Minocycline (Minocin)
Biologic drugs are the newest drugs for RA. They are either injected under the skin or directly into a vein. They work by neutralizing one of the immune system’s signals (TNF) that lead to inflammation and joint damage.
- Abatacept (Orencia)
- Adalimumab (Humira)
- Anakinra (Kineret)
- Certolizumab (Cimzia)
- Etanercept (Enbrel)
- Etanercept-Szzs (Ereizi)
- Golimumab (Simponi, Simponi Aria)
- Infliximab (Remicade)
Rituximab (Rituxan) and Tocilizumab (Actemra) are also biologics, but they do not block TNF.
Other drugs used to combat RA include:
- Azathioprine (Imuran)
- Cyclosporine (Neoral)
- Tofacitinib (Xeljanz)
DMARDs are sometimes started one at a time and increased gradually to minimize side effects. It can take more than one DMARD to get control of active rheumatoid arthritis. The goal is to reduce both medication side effects and rheumatoid arthritis disease activity.
Your physician may also prescribe splinting, which can help support the joint to ease the stress placed on it from frequent use and everyday activities. Splints are typically worn during periods when the joints hurt and small enough to allow use of the hand when they are worn.
Arthritis surgery treatments
If nonsurgical treatment fails to give relief, surgery is usually discussed. Your Florida Orthopaedic Institute physician will recommend a surgical treatment that has a reasonable chance of providing long-term pain relief and return to function and tailored to your individual needs. If there is any way the joint can be preserved or reconstructed, this option is recommended.
If the damage has progressed to a point that the surfaces no longer work, a joint replacement or a fusion (arthrodesis) is performed. Joint fusions provide pain relief but stop joint motion. The fused joint no longer moves and the damaged joint surfaces are gone, so they cannot cause pain and other symptoms. The goal of this procedure is to provide pain relief and restore as much function as possible.
After any joint reconstruction surgery, there is a period of recovery. Often, you will be referred to a trained hand therapist who can help you maximize your recovery. You may need to use a post-operative splint or cast after surgery. This helps protect your hand while it heals.
Videos
Related specialties
- Basal Joint Surgery
- Carpal Tunnel Syndrome
- De Quervain's Tenosynovitis
- Dislocated Finger
- Distal Radius Fracture (Broken Wrist)
- Dupuytren’s Disease
- Flexor Tendonitis
- Fractured Fingers
- Functional Nerve Transfers of the Hand
- Ganglion Cysts
- Hand & Finger Replantation
- Hand Nerve Decompression
- Hand Skin Grafts
- Nerve Pain
- Peripheral Nerve Surgery (Hand) Revision
- Revascularization of the Hand
- Sports Wrist & Hand Injuries
- Sprained Wrist
- Sudden Acute Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of the Hand
- Thumb Ulnar Collateral Ligament Injuries
- Trigger Finger
- Ulnar Neuritis
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
