Superior care from orthopedic hand specialists
Treatments for hand & wrist pain
The hand and wrist are an interconnected system of bones, joints, ligaments, tendons, and muscles that work together in a variety of positions hundreds of times a day. Because of their complexity and frequent use, it’s important to see an orthopedic hand specialist when pain interferes with your quality of life.






Learn more about
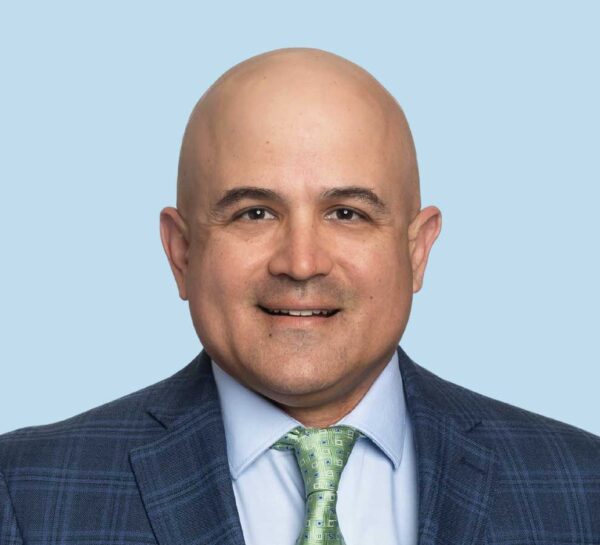
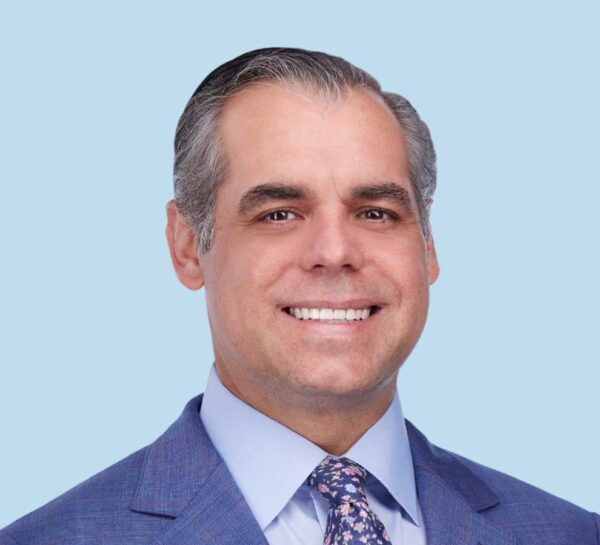
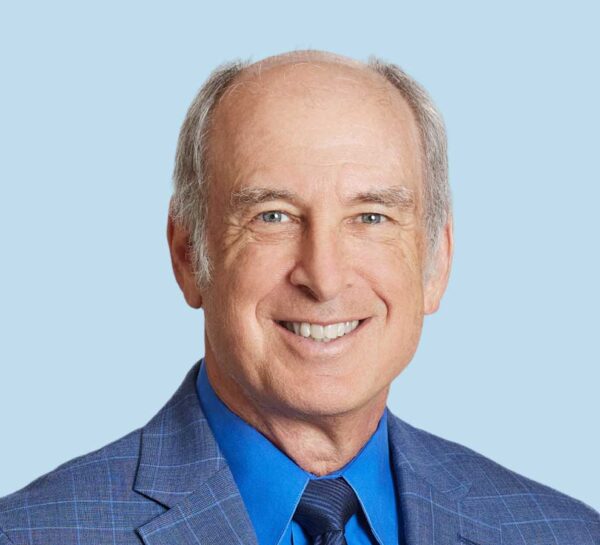
Orthopedic hand & wrist care team















Common hand & wrist conditions
Our highly reputable orthopedic hand and wrist specialists have extensive expertise in the causes of hand and wrist-related conditions, including the following:
- Carpal Tunnel Syndrome
- Colles’ Fractures (Broken Wrists)
- De Quervain’s Tenosynovitis
- Dupuytren’s Disease
- Finger Dislocations
- Flexor Tendonitis
- Fractured Fingers
- Fractured Wrists
- Ganglion Cysts
- Rheumatoid Arthritis of the Hand
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Thumb Ulnar Collateral Ligament (UCL) Injuries
- Trigger Finger
- Ulnar Neuritis
- Wrist Sprains
- Wrist Tendonitis
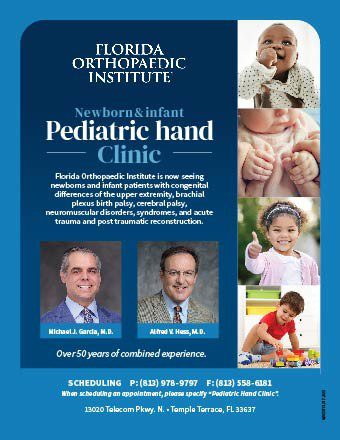
Learn how to schedule an appointment for newborn and pediatric hand treatment and reconstruction.
“The first time I got back to fishing, I was able to grip it, reel it in and cast it out. I love fishing. It’s like therapy. I just started fishing again like I used to.” Briant Cummings | Hand Replant
Treatments from orthopedic hand specialists
The fellowship-trained hand and wrist physicians at Florida Orthopaedic Institute are the leading providers of treatments for these intricate body parts, including:
Basal joint arthritis makes it difficult to grip and hold or twist objects between the thumb and fingers. It can be difficult to perform simple tasks, such as turning a doorknob, opening a jar and pinching or gripping an item. Although it may be successfully treated with nonsurgical options such as medications, severe cases of basal joint arthritis usually need surgery. Basal joint surgery removes and rebuilds the damaged basal joint.
When a nerve injury results in loss of muscle function or sensation, a functional nerve transfer is a surgical technique that is used to restore lost function and sensation. Nerves with less important roles or branches of a nerve that perform redundant functions are surgically transferred to the nerve area that has been damaged. The goal of a functional nerve transfer is to restore as much of the nerve’s sensation and function as possible.
Hand and finger replantation is the reattachment of a finger or hand that has been completely cut from someone’s body. The goal of this type of surgery is to give the patient back as much use of the injured area as possible. Your surgeon may offer to clean, smooth and cover the cut end (called a completion or revision amputation replantation) if the detached part is too damaged.
Nerve decompression surgery alleviates pressure on a nerve by opening narrow spaces to give the nerve more room or removing whatever is pressing on the nerve, or both. Due to the surrounding skeletal structure, some nerves are more prone to compression than others.
Hand skin grafts are used to treat skin damaged by burns, infection, or other injuries. Sheets of healthy skin are removed from one part of the body (the donor site) and placed on the damaged hand. If possible, healthy skin is taken from areas not easily seen or that are usually covered by clothes. There are two primary types of hand skin grafts: split-thickness skin graft (STSG) and full-thickness skin grafts. A split-thickness skin graft removes the epidermis (the top layer of the skin), as well as a portion of the dermis (the deeper layer of the skin). Full-thickness skin grafts use all the epidermis and dermis from the donor site. They are generally used for small wounds on highly visible parts of the body, as they blend in with the skin around them for a better cosmetic outcome.
Peripheral nerve injuries happen to more than 1.4 million Americans every year, with nearly 900,000 needing surgical intervention. In the past, surgeons have used the patient’s nerves from another part of their body to repair the damage. Surgeons at Florida Orthopaedic Institute are pioneering nerve pain solutions with new products from AxoGen.
Hand-related nerve damage can be caused by traumatic injuries, underlying illnesses like diabetes, immune system deficiencies, bacterial or viral infections, tumors or kidney and liver problems. Repeated exposure to toxic chemicals, alcoholism, chronic use of certain medications, and certain vitamin deficiencies can also cause hand-related nerve damage. If nonsurgical methods do not relieve nerve pain, an orthopedic hand and wrist specialist at Florida Orthopaedic Institute can provide peripheral nerve surgery.
Revascularization is the restoration of blood flow (perfusion) to a body part or organ that has suffered a restriction in blood supply to tissues (ischemia), causing a shortage of oxygen needed by your cells. In hand revascularization, an experienced and skilled hand surgeon repairs injured or damaged blood vessels to fix damaged tissue and restore blood flow to as normal a level as possible.
Targeted muscle reinnervation (TMR) is a surgical procedure that gives amputees easier, more intuitive prosthesis control. The nerves to spare muscles of an amputated patient are cut and/or deactivated (denervated), then reinnervated with residual nerves of the amputated limb. EMG (electromyography) signals of the targeted muscle can be used to drive motorized prosthetic devices. The reinnervated muscles serve as biological amplifiers of the amputated nerve motor signals, allowing for better control of sophisticated prosthetic arms.
Tendon transfers of the hand restore lost hand function after the loss of muscle or tendon function from a nerve injury (cut, stretched, or torn nerve) or muscle injury (trauma, rheumatoid arthritis). Tendon transfers are also used for neuromuscular disorders (cerebral palsy, stroke, traumatic brain injuries, and spinal muscle atrophy) or congenital disabilities (infants born without certain muscle functions). Tendon transfer of the hand is also used when a muscle has ruptured or been lacerated and cannot be repaired.
WALANT (wide awake local anesthesia no tourniquet) is an operating technique that uses two medications (lidocaine and epinephrine) for some types of hand and wrist surgeries in a safe and painless manner. This technique eliminates the use of tourniquets and general anesthesia. WALANT has many advantages, including no preoperative testing, no costs associated with anesthesia, no need for an IV and a lower overall cost.
Wrist arthroscopy is a minimally invasive technique which can be used for diagnostic purposes as well as for therapeutic interventions. First introduced in 1979, wrist arthroscopy became accepted as a diagnostic tool around the mid-1980s. Wrist arthroscopy utilizes a small fiber optic instrument called an arthroscope that allows the surgeon to see inside the joint without making large incisions into the muscle and tissue.



