Basal joint arthroplasty
Arthritis is a condition that irritates or destroys a joint. Although there are several types of arthritis, the one that most often affects the joint at the base of the thumb (the basal joint) is degenerative or “wear-and-tear” arthritis (osteoarthritis). While there are nonsurgical ways to treat this condition, basal joint surgery is the most effective way to treat basal joint arthritis.
Anatomy
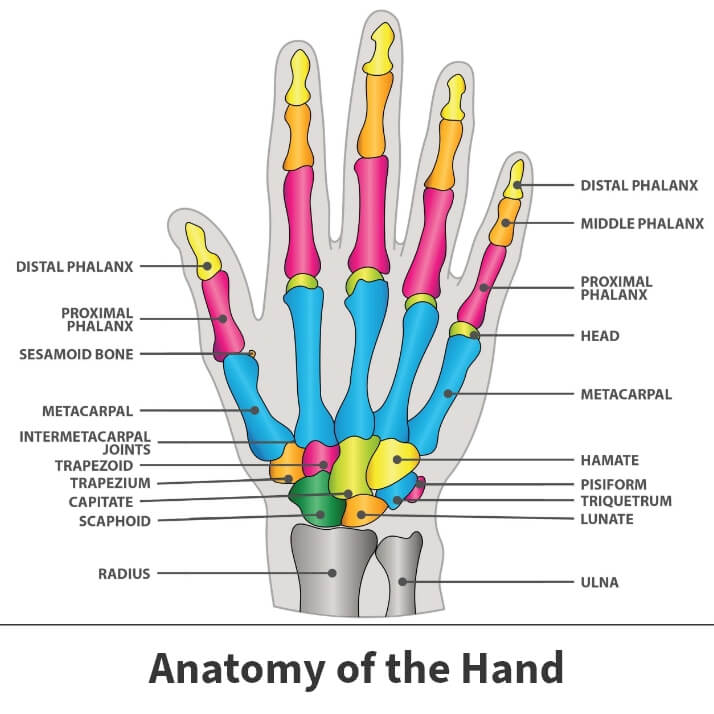
The thumb has two bones. The first bone (distal phalange) extends from the tip of the thumb to the knuckle. The second bone (proximal phalange) extends from the knuckle to the base of the thumb. This is the area of webbing between the thumb and the first finger. The thumb connects with the first metacarpal hand bone.
About
Arthritis of the thumb, also known as basal joint arthritis, occurs when the cartilage of the thumb joint wears away from the bone. Usually this cartilage acts as a cushion between the bones of the joint. When it is worn away, the direct contact and friction between the bones cause pain, swelling, decreased strength, and limited range of motion.
While cartilage usually covers the ends of the bones and allows them to move smoothly, arthritic joints have deteriorated cartilage that does not protect the bones. Without this protection, the bones rub against each other. Basal joint arthritis causes pain in the base of the thumb when gripping, grasping, or pinching an object, or when applying force.
Basal joint arthritis usually occurs because of an injury or general overuse. Patients who have experienced prior fractures or injuries to the thumb joint may be more vulnerable to developing this condition. The basal joint can be more susceptible to arthritis than other joints because it is used so frequently. Basal joint arthritis is also more common in women than men, and usually occurs over the age of 40. Some research suggests that it may be a genetic condition.
Symptoms
Symptoms of basal joint arthritis include:
- Swelling
- Stiffness
- Pain during sleep or when the thumb is not moving
- Tenderness
- Decreased strength
- Decreased range of motion
- Bony joint appearance
Diagnosis
Your Florida Orthopaedic Institute physician will take a look at your symptoms and overall medical history, followed by a physical examination. One of the tests used during the examination of the hand involves holding the joint firmly while moving the thumb. If pain results or a grinding sound is heard, it is an indication that the bones are rubbing directly against each other.
Additionally, your physician may decide also to take an X-ray of your thumb to determine whether there is any deterioration within the joint. X-rays can also show if bone spurs or calcium deposits have developed.
Treatment
Basal joint arthritis is typically initially treated with a combination of nonsurgical treatments, including the use of non-steroidal anti-inflammatory drugs to help with pain and swelling. Corticosteroid and biologic injections are also often used to help symptoms. Wearing a splint is also used to support the thumb and limit movement. But severe cases of basal joint arthritis usually need surgery to relieve pain and other symptoms.
Surgical treatment
Several surgical procedures are used to treat basal joint arthritis. These procedures include:
- Joint fusion (arthrodesis) – This procedure permanently fuses together the bones in the basal joint, increasing stability and reducing pain.
- Joint suspension (arthroplasty) – During this the trapezium bone with arthritis is removed and one of various techniques is used to keep the metacarpal bone in good position.
- Joint nano (arthroscopy) – This procedure allows for minimally invasive evaluation of the joint with removal of synovitis and is for earlier stage arthritis.
- Joint denervation – This procedure may be offered to remove painful sensory innervation to the joint.
There are many different ways to treat thumb basal joint arthritis surgically and your Florida Orthopaedic Surgeon will discuss these in more detail with you.
Recovery
After undergoing basal joint surgery, you will need to wear a cast or splint over the thumb and wrist for up to six weeks. Hand therapy is initiated soon after surgery to help you regain motion and strength. Recovery may take a few months or longer. Complete recovery from basal joint surgery may take up to six months.

Videos
Related specialties
- Carpal Tunnel Syndrome
- De Quervain's Tenosynovitis
- Dislocated Finger
- Distal Radius Fracture (Broken Wrist)
- Dupuytren’s Disease
- Flexor Tendonitis
- Fractured Fingers
- Functional Nerve Transfers of the Hand
- Ganglion Cysts
- Hand & Finger Replantation
- Hand Nerve Decompression
- Hand Skin Grafts
- Nerve Pain
- Peripheral Nerve Surgery (Hand) Revision
- Revascularization of the Hand
- Rheumatoid Arthritis of the Hand
- Sports Wrist & Hand Injuries
- Sprained Wrist
- Sudden Acute Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of the Hand
- Thumb Ulnar Collateral Ligament Injuries
- Trigger Finger
- Ulnar Neuritis
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
