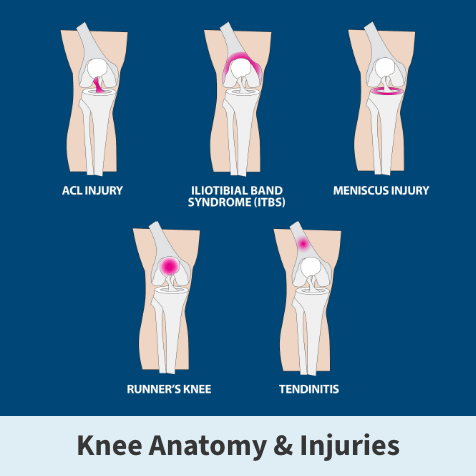
ACL injuries
Anterior cruciate ligament tears and sprains
Did you hear a “popping” noise or feel a snap in your knee after twisting or unnaturally moving it? You might have torn or sprained your anterior cruciate ligament (ACL). Instances of ACL injuries are especially high in athletes. Still, they can happen to just about anyone during everyday activities, such as after a bad fall or serious car accident.
ACL sprains and tears are the most frequently injured ligament in the knee, accounting for nearly half of all total knee injuries. In fact, in the U.S. alone, about one in every 3,500 people experiences an ACL tear each year, leading to around 400,000 ACL reconstruction surgeries annually.
No matter the cause, any knee injury disrupts your life and makes it hard to get around. Florida Orthopaedic Institute’s team of experienced surgeons and rehabilitation specialists helps patients across central Florida and beyond with convenient, comprehensive care for all ACL knee injuries, from diagnosis and treatment to rehabilitation and prevention.
Keep reading for in-depth information about tears and sprains from our experts, covering what you need to know about ACL injury symptoms and their causes, treatment options, and recovery strategies. Plus, check out the FAQ at the end of this page for answers to popular questions and tips for preventing ACL injuries.

ACL tears and sprains overview
Depending on the type of injury, treatment options for ACL tears and sprains can range from non-surgical rehabilitation to surgical intervention (reconstruction or possible repair), which aims to restore full knee function.
Factors influencing the treatment approach include injury severity, knee anatomy, overall health, activity level, and recovery goals.
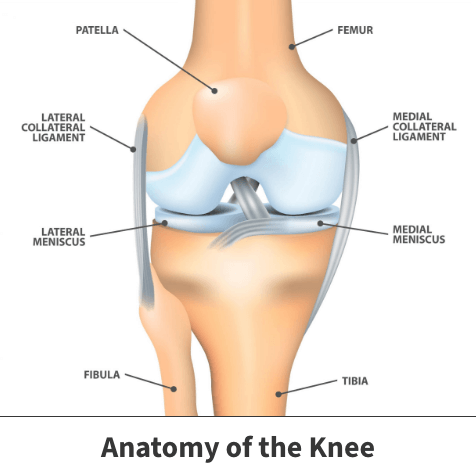
Knee anatomy and its ACL ligament
The knee is a hinged joint with four main parts: ligaments (including the ACL), bones, cartilage, and tendons. The thigh bone (femur), shin bone (tibia), and kneecap (patella) meet to form the entire knee joint, and the kneecap helps protect the front of this joint.
Ligaments connect one bone to another to help keep our joints stable. Think of the ligaments as a rope with a fixed length. The knee has four primary ligaments, which connect the thigh bone (femur) to the shin bone (tibia):
- Collateral ligaments (medial collateral ligament and lateral collateral ligament)
- Cruciate ligaments (anterior cruciate ligament and posterior cruciate ligament)
Collateral ligaments
The knee’s collateral ligaments control side-to-side stability and protect the joint against sudden movements. The medial collateral ligament is on the inside of the knee, while the lateral collateral ligament is on the outside.
Cruciate ligaments
The knee has two cruciate ligaments, the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), which control primarily front-to-back and rotational stability.
Anterior cruciate ligament
This ligament runs diagonally in the middle of the knee and helps keep the shin bone (tibia) from sliding forward in the thigh bone (femur). It also provides rotational stability by preventing the tibia from rotating on the femur. ACL ligament tears usually result in the knee feeling unstable and cause random buckling or giving way with any twisting, pivoting or jumping activities.
Posterior cruciate ligament
This ligament mirrors the ACL. It also runs diagonally but in the opposite direction of the ACL. The result is a crossing of the two ligaments, forming an “X” in the middle of the knee. This is why they are named cruciate ligaments. The primary function of the PCL is to keep the shin bone from sliding backward to the thigh bone.
Cartilage
Articular and meniscus are the two main types of cartilage in the knee.
Articular cartilage
Articular cartilage is a layer of specialized cartilage that covers the bony ends of nearly all joints in the body, including the knee. It provides a perfectly smooth surface so that joints move without friction and pain. Arthritis occurs when the articular cartilage wears away; if severe enough, it may require a knee replacement.
Meniscus
The meniscus is a type of specialized cartilage found in the knee. It is horseshoe-shaped and located between the shin and thigh bones. Each knee has a meniscus on the inside (medial meniscus) and outside (lateral meniscus).
The meniscus has many functions but primarily acts as a shock absorber for the knee. It protects the articular cartilage by helping to dissipate load across the joint during weight-bearing activities like walking and running.
What are ACL injuries?
An ACL injury means some damage has been done to this key ligament that helps stabilize your knee joint.
These injuries often happen when the ligament is overstretched or torn due to a sudden stop, quick and unexpected change in direction, or direct impact on the knee. This is why knee joint injuries are common in high-demand sports like soccer, football, and basketball.

Types of ACL injuries and how they’re classified
Medical professionals refer to a sprain as any injury to a ligament, so damaging an ACL would be classified as a sprain, which occurs when the ligament fibers are overstretched or torn. These injuries can vary quite a bit in severity. That’s why medical professionals use a grading system to help assess the extent of the damage:
ACL injuries are graded on a “severity scale” based on different levels of damage or seriousness, using the following three categories:
- Grade 1 ACL injury: Minor damage, mild stretching
- Grade 2 ACL injury: Stretched and partially torn
- Grade 3 ACL injury: Completely torn in half and no longer providing stability
Grade 1 injury
This is the mildest form of an ACL injury, where the ligament fibers are slightly overstretched, resulting in minor damage. While you may experience mild discomfort, the ligament remains intact, and the knee can function normally. However, the joint may feel tender with specific movements until the healing process is complete.
Grade 2 injury
This level indicates a partial tear of the ACL (the ligament is stretched and damaged to a greater extent, possibly leading to a loss of stability in the knee). If you have a Grade 2 sprain, you may find it difficult to pivot or change direction, as the knee may buckle or feel unsteady during these actions. This sprain often requires more time to heal and may benefit from rehabilitation to regain full function. Surgery may be indicated if conservative treatment fails.
Grade 3 injury
Grade 3 is the most severe form of ACL injury. It means the ligament is completely torn or ruptured. This type of injury usually results in significant pain, knee swelling, and instability. Your knee joint can no longer provide stability, making running, pivoting or jumping nearly impossible without support.
ACL surgery is often necessary to repair a Grade 3 sprain, followed by extensive rehabilitation to restore strength and function.
Tibial spine avulsion ACL injuries
Tibial spine avulsion is another injury that doesn’t technically fall under the standard ACL damage grading scale. This injury happens when the ACL ligament pulls away a portion of the tibial spine (the bony area of the shin where the ACL is attached).
We see this type of injury more frequently in children and adolescents because their bones are still developing and are more vulnerable to fractures than a complete ligament tear. Unlike a typical ACL tear, a tibial spine avulsion involves damage to the bone attachment of the ACL on the tibia rather than just the ligament itself.
Because tibial spine avulsion injuries aren’t part of the ACL grading system, they’re considered a distinct type of injury that may require different treatment approaches, often involving surgical intervention to reattach the bone fragment to restore normal ACL tension.
Understanding the severity of ACL injuries is essential to determine the right treatments and ensure recovery.
What causes ACL injuries?
While athletes are most vulnerable to ACL tears and sprains, they can happen due to contact and non-contact injuries. Some of the most common causes of ACL knee injuries include:
- Sports and high-risk activities
- Direct trauma
- Non-contact rotational movements
Sports and high-risk activities
Athletes or adventurers participating in sports and activities involving rapid movements (such as short and sudden stops, sharp turns, and leaps) are significantly more likely to experience ACL injuries.
Some sports (like football, basketball, soccer, and skiing) place high demands on your knees. Research suggests that 70% of sports knee injuries, like ACL sprains and tears, are non-contact, occurring during these types of sudden movements, while the remaining 30% result from direct trauma during contact sports.
Read how Dr. Glasser helped Zach return to the field after a soccer ACL tear
Direct trauma
Some ACL tears are caused by traumatic, direct impacts to the knee during contact sports (e.g., football tackles) or serious accidents (e.g., car collisions).
In these instances, force exerted directly onto the knee may tear the ligament. Contact-related ACL knee injuries often lead to other kinds of joint damage, such as meniscus tears, fractures, and ligament damage, further complicating the recovery process.
Non-contact movements
Many ACL injuries result from simple, everyday accidents. These, too, can happen through sudden stops, quick pivots, or improper landings from steps or jumps. Poor landing and abrupt stopping can increase the risk of overstretching or tearing the ACL.
More specifically, your ACL can be injured from:
- Rapidly changing direction
- Deceleration coupled with cutting, pivoting, or sidestepping moves
- Suddenly stopping
- Awkward or incorrect landings from a jump
- Out-of-control play
- Direct contact or collision (like a football tackle or car accident)

Signs you might have injured your ACL
Swelling may occur immediately or within a few hours after an ACL tear. Sometimes, the swelling and pain resolve on their own over time. However, you risk causing further damage to your knee’s cushioning cartilage (meniscus) if you return to sports with an unstable knee.
Other typical symptoms of an injured anterior cruciate ligament include:
- A “popping” noise – This is a common and often alarming signal at the moment of injury that you’ve torn or overstretched your knee’s ACL.
- Your knees give out (instability) – Many people describe this sensation associated with an injury to the ACL as their knee joint suddenly feels unstable.
- Loss of range of motion – Instability caused by an injured ACL can cause significant swelling in the joint, making it challenging to straighten or bend your knee joint fully.
- Pain & swelling – Significant bone bruising in the tibia and femur usually occurs when the knee joint is translated and rotated during an ACL rupture. Bleeding into the joint from the torn ACL results in fluid accumulation within the joint. This causes significant pain and swelling shortly after most ACL tears.
- Discomfort while walking or putting weight on the leg – Even though the pain and swelling may subside on their own over time, the underlying damage remains and can make everyday activity a struggle.
Factors that increase the chance of ACL injury
Some individuals are more at risk than others for experiencing ACL injuries, which are commonly associated with the following risk factors:
- Gender,
- Age,
- Involvement in sports,
- Knee anatomy,
- Environmental factors and
- Previous injuries to the ACL.
Gender
Female athletes are at an alarmingly higher risk than males, especially in sports like soccer and basketball. This increased risk in women is believed to be linked to several factors, such as differences in muscular strength, neuromuscular control, pelvis and lower leg alignment, space available for the ACL (notch stenosis), the effects of estrogen, and loose ligaments in general.
Age
ACL injuries are more common in younger, active individuals, especially those between the ages of 15 and 45, who are more likely to take part in high-risk sports and strenuous activity.
Involvement in sports
Sports that involve sudden stops, quick pivots, and jumps—like football, basketball, soccer, and skiing—are high-risk activities for ACL knee injuries. Athletes in these sports often place excessive, consistent strain on their knees, increasing their chances for damage.
Knee anatomy
Certain anatomical factors can increase a person’s risk of tearing, such as:
- ACL ligament size,
- Leg alignment,
- Increased looseness of the knee’s normal ligaments and
- Decreased space in the knee for the normal ACL.
Environmental factors
Playing surfaces like artificial turfs and concrete courts, footwear, and weather conditions can also contribute to the risk of ACL injuries, as they affect traction and stability during play.
Previous injuries to the ACL
Individuals who have already torn their ACL are at greater risk of reinjury, particularly if they return to high-intensity activities without proper rehabilitation.
Other factors
Other factors include poor conditioning, weak core muscles, muscle imbalances (quad-to-hamstring ratio), and direct contact.
It’s important to note that half of ACL injuries don’t occur in isolation. When the ACL is torn, other structures in the knee, such as the meniscus, articular cartilage, or even other ligaments, are often damaged as well.
A well-known combination of injuries is called the “unhappy triad,” often seen in football players and skiers. In this triad, the ACL, MCL, and medial meniscus are all damaged in the same incident. This triad is particularly serious and usually requires surgical intervention and extensive rehabilitation.
Diagnosing ACL injuries
A detailed and thorough history and physical exam are critical to accurately diagnosing. It is also important to understand your lifestyle and goals for future activities.
One key test we perform during the physical exam is the Lachman Test. This test allows knee specialists to determine whether the ACL is completely torn. Additional physical exam maneuvers evaluate all structures in the knee, including other ligaments, tendons, meniscus, articular cartilage, neurovascular status, etc.
Although X-rays don’t show ACL tears, they provide valuable information and are typically obtained during the initial visit. This allows us to evaluate many factors that are important when treating ACL injuries, such as associated fractures, arthritis, leg alignment, the status of the growth plate in younger patients, and bony changes from any prior surgeries.
MRI scans are obtained to visualize all the additional soft tissue structures that don’t appear on X-rays. This includes ligaments, tendons, meniscus and articular cartilage, muscles, nerves, arteries, etc.
How knee specialists help
If not identified and treated quickly, ACL tears can worsen. Additionally, these injuries can negatively impact other knee structures, leaving you at greater risk of developing other painful and potentially life-impacting issues.
Rehabilitation and proper treatment are critical to recovery. Attempting to return to physical activities or sports without adequate healing can lead to further damage, especially to the meniscus, the cartilage that cushions the knee joint. If the knee remains unstable, the risk of long-term complications, including chronic pain and arthritis, increases dramatically.
If you have symptoms pointing to an ACL injury as the cause for knee pain that hasn’t improved in 48 hours, don’t wait to start the recovery process. See a sports medicine orthopedic expert to quickly determine what is causing your symptoms, explore non-surgical and surgical options, and begin the right course of treatment.
ACL tear treatments
An ACL tear diagnosis can be stressful. That’s why the orthopedic specialists at Florida Orthopaedic Institute take a comprehensive approach to treating ACL knee injuries, accounting for factors like age, overall health, the severity of the injury, and activity level.
For example, if you’re a younger athlete with instability on examination and a complete ACL tear who wants to get back to sports quickly, we typically recommend surgery. On the other hand, if you’re in a certain age demographic, have minimal symptoms, and lead a less active lifestyle, you may be able to avoid surgery and instead focus on less invasive, non-operative treatments.
At an appointment with an FOI knee specialist, you can expect a thorough assessment of your injury and a customized treatment plan. For instance, in the cases of partial tears, surgery isn’t always necessary. Physical therapy and ongoing check-ins with our orthopedic specialists may help you regain stability and prevent future issues.
However, an operation is typically required to restore knee function if the ACL is completely torn. It is also important to remember that ACL tears can sometimes affect other parts of the knee, such as the meniscus or cartilage. Close monitoring and follow-up care are critical to successful recovery and avoiding further complications.
Who are the best candidates for conservative ACL treatment?
Certain types of ACL injuries may be better suited for non-operative treatment. Specific examples of who might be a good candidate for non-surgical ACL injury treatment include someone who:
- Has a complete ACL tear, isn’t experiencing any pain or instability with daily activity, and participates in low-impact non-pivot sports like swimming and biking,
- Has a partial ACL tear and doesn’t have any instability on examination,
- Works in a sedentary job requiring little or no physical labor and not participating in at-risk activities or
- Is a less active, growing child with a partial tear, good stability, and no other cartilage damage.
While a torn ACL usually won’t fully heal without surgery, nonsurgical care can be a good option for older individuals or those with lower activity levels. The success of nonsurgical healing depends on several factors, including lifestyle, the extent of the injury, and the level of knee stability.
Physical therapy for ACL sprains is customized to each patient’s injury, helping to strengthen surrounding muscles and improve knee function.
Recovery from partial ACL tears may be possible without an operation. Rehabilitation can take at least three months. We recommend comprehensive follow-up care and physical therapy to monitor progress and address any remaining instability, helping our patients regain optimal knee function and determine if additional treatment is necessary.
What are the benefits of nonsurgical treatment?
The outcomes without surgery are generally less favorable for patients with a complete ACL tear. Many people may experience knee instability during everyday activities like walking, and athletes find it challenging to participate in sports involving cutting or pivoting movements. However, depending on their needs and the severity of their ACL injuries, some individuals may still function without having instability. A customized ACL brace may also provide additional stability for the injured knee.
The risk of living with an unstable knee that buckles or gives way is the potential for secondary damage. Repeated knee instability can cause meniscus and articular cartilage injuries, leading to long-term knee problems.
What’s involved in conservative treatment of ACL injuries?
If you are a candidate for non-conservative treatment, your Florida Orthopaedic Institute physician may recommend these nonsurgical options:
- Bracing to protect your knee from instability initially
- Crutches initially to help decrease pain, lessen swelling and prevent further damage until the acute inflammation resolves.
- Physical therapy to help restore function to your knee and strengthen the supporting muscles.
Surgery for ACL tears
In most cases, a patient will require surgery to fix the damaged ligament to restore normal knee function. There are two basic surgical options: repair and reconstruction. A small percentage of patients may be a candidate for ACL repair.
This involves using sutures to sew the torn ligament back to its attachment site on the femur and possibly adding a collagen implant (BEAR technique) to stimulate a more robust healing process. However, most ACL tears are not candidates for repair and are treated with a more traditional ACL reconstruction. This involves replacing the torn ligament with a tendon graft, usually taken from another area around the knee.
Popular grafts include a small portion of the patellar tendon, quadriceps tendon, or hamstring tendons. After removing the torn ACL, the graft is secured under tension at the anatomic bony attachment sites on the femur and tibia, restoring normal knee stability.
Here at Florida Orthopaedic Institute, surgery for ACL tears is performed outpatient using small incisions and arthroscopic techniques. This minimally invasive surgery allows for shorter operative times, less tissue damage, smaller scars, less pain and swelling, and a faster recovery. Any additional damage, such as meniscus tears or articular cartilage injuries, is addressed simultaneously.
Consult one of our orthopedic sports medicine physicians for more information about outpatient surgery options and recovery for treating ACL injuries.
Learn more about outpatient surgery
Deciding whether or not to have ACL surgery
If you’re an active adult whose job involves pivoting, turning, or performing heavy manual labor or if you play sports, surgery is usually the best option to regain full function and avoid long-term knee instability. However, the patient’s activity level and goals (more than age) play a significant role in whether or not surgery is recommended.

For very young children or adolescents, our surgeons may occasionally choose to delay ACL surgery until they are closer to skeletal maturity to avoid potential injury to the growth plates. However, in most cases, ACL surgery can be successfully performed with technique modifications to minimize the risk of growth-related issues.
You may also need surgery if there are other injuries involved, such as a meniscus tear. In fact, nearly half of meniscus tears can be repaired more effectively when done simultaneously with ACL reconstruction, leading to better long-term outcomes for the knee.
Discussing your situation with one of our orthopedic specialists can help determine the best path forward.
How are grafts used to rebuild a torn ACL?
During ACL reconstruction surgery, a tissue graft replaces the torn ligament. This graft undergoes remodeling as new tissue grows into and strengthens it. Athletes often wait nine months to a year before returning to unlimited sporting activity.
Where do grafts used for ACL reconstruction come from?
Grafts used for ACL reconstruction surgery can come from a few different places. If the graft is from your body, it’s called an autograft and involves taking a small portion of a normal tendon to replace your torn ACL. Popular options include:
- Patellar tendon autografts use the tendon that connects the kneecap (patella) to the shinbone (tibia).
- Hamstring tendon autografts are taken from the tendons at the back of the thigh (hamstring).
- Quadriceps tendon autografts come from the tendon that connects your thigh muscle (quadriceps) to the top of your kneecap (patella).
Alternatively, grafts called allografts can be sourced from certified tissue banks for ACL surgery. Options include the same tendons noted above and alternatives such as the Achilles tendon or posterior tibialis tendon.
At Florida Orthopaedic Institute, your surgeon will discuss the pros and cons of each graft option to determine which is best for you. It’s important to note that because the graft needs time to integrate and grow, it typically takes at least nine months or more before athletes can safely return to their sport following ACL surgery.
Are there any special considerations when treating pediatric ACL injuries?
Yes, because children and adolescents are still growing, surgery to repair a torn ACL must account for the presence of growth plates (the areas of developing cartilage near the ends of long bones). Performing ACL surgery in young patients requires techniques that avoid damaging these growth plates, as injury can lead to bone growth abnormalities and leg alignment issues.
At Florida Orthopaedic Institute, our sports medicine knee specialists have extensive experience treating pediatric ACL tears. We prioritize surgical techniques that respect the growth plates to ensure our younger patients’ short-term recovery and long-term well-being. We also work closely with families to determine the safest and most effective treatment options for their individual child’s ACL injury.
How to prepare for ACL injury surgery
ACL surgery can feel overwhelming, but being well-prepared can make a big difference in your recovery and peace of mind. At Florida Orthopaedic Institute, we’re here to support you every step of the way.
Before ACL injury surgery, you’ll need to do some work to ensure you have the smoothest possible recovery process.
Prepare mentally by speaking with your surgeon to get a clear picture of what to expect after your procedure. Ensure your home is set up to make getting around easier and rearrange furniture and rugs to minimize tripping hazards. You’ll also need to line up support to help you, as needed, with day-to-day tasks. Lastly, you’ll want to get your knee ready for surgery by strengthening it with exercises recommended by your surgeon (prehabilitation).
Doing this work in advance will give you the best chance for a successful surgery and a faster, more comfortable recovery.
ACL surgery preoperative instructions
Before undergoing ACL surgery, following a specific set of preoperative instructions is essential to ensure a smooth procedure and successful recovery. These steps help you prepare physically and mentally for surgery.
Key steps include stopping certain medications (like blood thinners) a few days before the procedure, fasting as instructed (usually starting the night before) and preparing your home for post-surgery mobility. You will also be advised to perform pre-surgery exercises (prehabilitation) to strengthen your knee and improve your recovery.
Florida Orthopaedic Institute provides clear guidelines to help minimize risks and prepare patients for a quicker, safer recovery. We also know that every patient is unique, so you’ll have ample time to discuss these steps with your orthopedic surgeon before the procedure.
Please contact our team if you have questions or need clarification on your pre-surgery steps. We’re here to support you every step of the way.
Potential complications from surgery for ACL injuries
ACL surgery has come a long way and is generally safe and highly effective in restoring knee stability and function. However, as with any surgical procedure, there are potential complications that patients with ACL injuries should be aware of. These risks are rare but can include:
- Infection: Any surgery comes with the risk of infection at the incision site or within the knee joint itself; however, these are extremely uncommon.
- Knee stiffness: Some patients may experience difficulty regaining full range of motion after surgery, which may require additional physical therapy or, in rare cases, a second procedure.
- Graft failure: If placed under excessive strain before fully integrating into the knee anatomy, the new ligament (graft) may not fully heal or could re-tear. Therefore, it is critical that you follow the rehabilitation protocol throughout your recovery.
- Blood clots: There is a minor risk of developing blood clots following surgery, especially in the legs. Your doctor will provide post-op instructions to reduce this risk.
- Nerve or blood vessel damage: Though extremely rare, damage to surrounding nerves or blood vessels can occur during the procedure.
At Florida Orthopaedic Institute, we take every precaution to minimize these risks and provide patients with the best care for ACL injuries. Discuss your concerns about potential complications with your surgeon and follow all postoperative instructions closely to ensure a successful recovery.

Rehabilitation after ACL injury treatment
Rehabilitation is critical to the recovery timeline for your ACL injury, whether you’ve had surgery or opted for nonsurgical treatment. A customized physical therapy program will help you regain strength, flexibility, and motion in your knee, ensuring that you can safely return to your daily activities.
After surgery, the initial focus of physical therapy is to decrease pain, lessen swelling and restore motion to the joint. Once the knee’s range of motion improves, the next phase emphasizes strengthening exercises to protect the new ligament and gradually increase the stress placed on the knee.
This is followed by adding functional drills to improve proprioception, balance, agility and endurance. If you are an athlete, the final phase of rehabilitation focuses on sport-specific movements. Objective measures, including isokinetic strength testing (biodex), vertical drop test, hop testing, etc., are also utilized to determine return to sport readiness.
At Florida Orthopaedic Institute, our rehabilitation programs are tailored to each patient, ensuring the best possible outcome and returning you to your pre-injury lifestyle.
Post-operative physical therapy benefits
Physical and occupational therapy is a key part of the recovery after surgery for an ACL injury. It helps restore strength and mobility to your knee, improves flexibility, reduces pain, and prevents complications down the road, like stiffness and aching.
By slowly increasing activity under the supervision of a physical therapist, you can ensure that your new ligament heals properly and that you can confidently return to your normal activities.
How long does physical therapy take during rehabilitation after surgery?
The amount of physical therapy needed after surgery for ACL injuries varies. For example, a patient with an ACL tear may require six to 12 months of physical therapy, with the early stages of their rehab focused more on restorative exercises for range of motion and the later stages targeting building strength and movement. This process can take longer for an athlete because additional work and strengthening are needed to re-enter sports.
Talk to your physical therapist regularly about your progress and goals to set expectations for each recovery phase.
Safe return to sports & sport-specific training
We recognize how important it is for an athlete to be able to safely and confidently return to their sport following ACL surgery. A fundamental part of post-op rehab for athletes with ACL injuries includes sport-specific training, which helps ensure the knee is strong, stable, and ready to handle the demands of the particular sport, whether it’s running, cutting, pivoting, or jumping.
This specialized physical therapy gradually reintroduces movements that mimic those you’ll do in your sport, allowing you to regain strength, balance, and agility to get you back on the field or court.
Is it possible to resume my previous sports activities after rehabilitation?
Yes! Returning to your sport after ACL rehabilitation is possible, but the timeline and success depend on a few important factors.
While nothing can be fully guaranteed, your ability to resume sports activities will largely depend on how well your knee heals, the strength and stability you regain during physical therapy, and—this one is essential—how committed you are to follow your custom rehab plan.
For many athletes, the recovery process takes 9 to 12 months, with specific training tailored to the demands of their particular sport.
Prevention of ACL injuries
While you can’t predict an injury, there are some steps you can take to help prevent ACL injuries. Building strength, improving balance, and practicing proper technique, especially during sports, are good ways to keep your knees healthy and prepared.
Exercises that focus on strengthening the muscles around your knee—like the quadriceps and hamstrings—can provide much-needed stability to the knee joint. In addition, core and pelvic muscle strengthening exercises are equally important. Practicing balance and agility are also helpful ways to train your body to handle quick changes in direction, which can cause ACL injuries.
Studies show that incorporating neuromuscular training into your routine can significantly reduce your risk of ACL injury. Also, invest in the proper footwear and gear for your sport and always warm up properly before beginning high-intensity activities.
We work closely with our patients to offer guidance on specific exercises and prevention techniques that can help keep their knees strong and healthy. These steps can go a long way toward protecting their ACLs and allowing them to continue participating in the activities they love.
Training & exercise tips
Proper training and exercise can help prevent ACL injuries and keep knees strong and healthy. Whether recovering from an existing injury or just looking to build strength, focusing on a mix of strength, flexibility, and balance is needed for the best results.
At Florida Orthopaedic Institute, we recommend exercises targeting the muscles around your core, pelvic girdle, and knee (quads and hamstrings). We also incorporate balance and agility drills to stabilize you during sudden, quick movements.
Here are some tips to help you stay safe and keep your knees in tip-top shape.
4 things you can do to reduce your risk of ACL injuries
Be mindful of your movements and maintain good physical habits to prevent damage to your ACL. Here are four practical steps you can take to help minimize your potential for ACL sprains or tears:
- Use good technique and wear proper footwear: We can’t stress enough how important it is to use the right form, whether playing sports or working out. Be aware of your movements, especially during any activity that involves jumping or pivoting, and always wear footwear that offers good support and stability.
- Warm up/stretch before intense activity (and avoid activity when overtired): Prepare your body for exercise with a proper warm-up session and stretching to help increase blood flow and flexibility, reducing the chance of injury. Avoid pushing yourself too hard when you’re losing steam, as tired muscles can lead to a greater risk of making movements that cause ACL injuries.
- Mix core strengthening exercises with conditioning/flexibility training: A strong core and flexible muscles go a long way toward protecting your knees. Try incorporating strengthening exercises and flexibility work into your routine to help improve stability and reduce strain on your ACL.
- Get advice from a sports medicine specialist: No two bodies are alike; therefore, seeking guidance from a professional who can evaluate your needs and provide personalized tips is always helpful. A sports medicine rehabilitation specialist can create a tailored training plan to keep your knees healthy and injury-free.

FAQs about ACL injuries
People with sprains and tears in their ACLs have many different concerns. Below, we’ve gathered answers to some of the most common questions we hear from our patients.
Not all ACL tears are the same, but you’ll probably hear a “pop” and feel like your knee just gave out on you. This is usually followed by pain and swelling in the knee area and difficulty bearing weight or continuing activity. The knee will become unstable, especially during pivoting movements or sudden changes in direction.
Yes, without proper attention and treatment, injuries like complete ACL tears can lead to long-term knee complications. This includes recurrent instability with possible additional cartilage damage, chronic pain, and an increased risk of developing arthritis later in life.
No two injuries are exactly alike, but generally, the recovery from an ACL tear can take anywhere from 9 to 12 months before a person can return to full activity, including sports. Healing can involve non-surgical treatment or surgery, but in both cases, a dedicated physical therapy program is needed to restore strength and stability.
The short answer is yes: Non-surgical treatments like physical therapy can sometimes improve knee function, particularly for less active individuals or those with partial tears. However, a complete ACL tear typically requires surgery to restore the knee’s stability fully. This is especially true for athletes or those with active lifestyles.
Female athletes are more prone to ACL tears due to a combination of factors, including body mechanics, muscle imbalances, ligamentous laxity, and hormonal differences. Anatomically, women tend to have a wider pelvis, which ultimately affects knee alignment, and their landings during sports can put more stress on the ACL.
Athletes who return to high-impact sports too quickly are far more likely to experience a re-tearing of their ACL. Improper rehabilitation, muscle weakness, or failure to follow recovery protocols and a physical therapy program also increase the likelihood of re-injury. That’s why adhering to a comprehensive recovery plan is crucial to reducing this risk.
FOI sports medicine physicians recommend neuromuscular training. Beneficial exercises include core strengthening, resistance training, speed and agility training, plyometrics, balance exercises, and stretching. Practice proper landing mechanics. A good warm-up routine is essential. Avoid overtraining, get enough sleep, and follow a healthy diet with adequate hydration.
Pickleball for seniors: 10 tips for pain-free play
Related specialties
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
- Total Knee Replacement Surgery