Anatomy
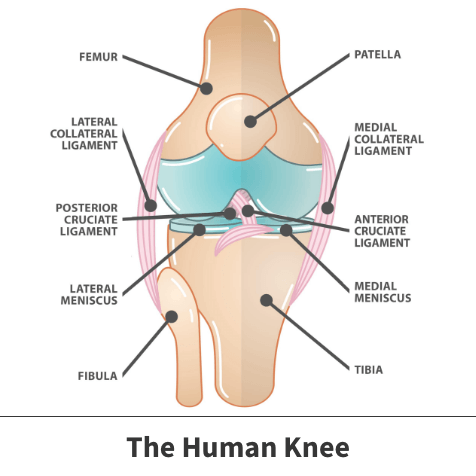
Your knee joint has three bones:
- Thighbone (femur)
- Shinbone (tibia)
- Kneecap (patella)
The ends of the thighbone and shinbone, as well as the back of the patella, are covered with articular cartilage, a slippery substance that helps your knee bones glide smoothly across each other when bending or straightening the leg.
The menisci are two wedge-shaped pieces of cartilage that act as “shock absorbers” between your thighbone and shinbone. Unlike the articular cartilage, menisci are strong and elastic. They help cushion the joint and keep it stable. There are two menisci in each knee, one on each side of the joint.
Another important part of the knee joint is the synovium. The knee joint is surrounded by a thin lining that surrounds the knee joint called the synovium. The synovium releases a fluid that lubricates the cartilage and reduces friction during movement.
Ligaments connect bones to other bones and the four main ligaments in your knee act like strong ropes to hold the bones together and keep your knee stable. Two collateral ligaments are on either side of the knee. Two cruciate ligaments are inside the knee joint and cross each other to form an “X.”
About
There are several ways that the meniscus is torn. Tears are classified by how they look, as well as where the tear occurs in the meniscus. Common tears include:
- Bucket Handle
- Degenerative
- Flap
- Radial
Meniscus tears occur along with other knee injuries, such as anterior cruciate ligament tears, especially in sports. If players squat and twist the knee or have direct contact (like a tackle), it can cause a meniscus tear.
Degenerative meniscus tears occur more often in older people. Cartilage wears thin and weakens over time and is more prone to tears. When the menisci have weakened with age something as simple as an awkward twist when getting up from a chair can be enough to cause a tear.
Find out more about the signs of meniscus tears and other pickleball knee injuries.
Symptoms
People sometimes feel a “pop” when they tear a meniscus. With a tear, most people can still walk on their injured knee (and many athletes keep playing) but over two to three days the knee will become stiff and swollen.
The most common symptoms of a meniscus tear are:
- Catching or locking of the knee
- Not able to move the knee through a full range of motion
- Pain
- Sensation that the knee is “giving way”
- Stiffness
- Swelling
Without care, a piece of meniscus may come loose and drift into the joint causing the knee to pop, slip, or lock.

Diagnosis
During a physical examination, your Florida Orthopaedic Institute physician will ask about your symptoms and medical history. They will check for tenderness along the joint line where the meniscus is located, as tenderness often signals a tear.
Another test for meniscus tears is the McMurray test where your doctor bends your knee, then straightens and rotates it. This test puts tension on a torn meniscus. If a meniscus tear is present, the movement will cause a clicking sound each time the doctor does the test.
Because other knee problems can have similar symptoms, your doctor may use imaging tests to help confirm the diagnosis. Testing can include X-rays and magnetic resonance imaging (MRI) which generates better images of the soft tissues of your knee joint.
Treatment
Your treatment will depend on the type of tear you have, its size, and location. Your age, activity level, and any related injuries are factors in a treatment plan.
The outside one-third of the meniscus has a rich blood supply. A tear in this area may heal on its own. The inner two-thirds of the meniscus lacks a blood supply so tears in this area cannot heal on their own. Because the pieces cannot grow back together, and often occur in thin, worn cartilage, tears in this area usually need surgery.
Nonsurgical treatment
The Florida Orthopaedic Institute’s philosophy is to first try all appropriate nonsurgical methods to increase mobility and function. This may include medication, bracing, injections or physical therapy. Then, and only then, do we suggest surgery.
If the tear is small and on the outer edge of the meniscus, it may not need surgical repair as long as your symptoms go away and your knee is stable.
Your Florida Orthopaedic Institute physician may recommend RICE: Rest, Ice, Compression, and Elevation.
Non-steroidal anti-inflammatory medicines (NSAIDs) like aspirin and ibuprofen (Motrin, Advil) can help reduce pain and swelling.
Your doctor may also recommend an injection into the knee joint for quick relief of pain and inflammation.
Surgical treatment
If nonsurgical treatments fail to relieve your symptoms, arthroscopic knee surgery may be suggested. Knee arthroscopy allows doctors to view the knee joint without making large cuts (incisions) through the skin and other soft tissues. These small incisions are also called portals.
A miniature camera (called an arthroscope) is inserted through a small incision provides a clear view of the inside of the knee. The image projected on a screen helps to diagnose the problem. Then miniature surgical instruments are inserted through other incisions to repair or trim the tear.
Because the arthroscope and surgical instruments are small, they are inserted through very small incisions, much smaller than the larger incisions needed for open surgery. This means less pain for patients, less joint stiffness, and shorter recovery times.
Specialized instruments are used to shave, cut, grasp, and repair. Special devices are used to anchor stitches into bone.
Most knee arthroscopy procedures last less than an hour, with the length dependent on the findings and treatment needed.
Read the questions you should ask your doctor about meniscus tears.
Videos
Related specialties
- ACL Injuries
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
- Total Knee Replacement Surgery
