Shin splints
Shin splints (medically termed medial tibial stress syndrome) are a common problem that occurs when exercising. Whether old or young, shin splints can happen to anyone who is participating in physical activity. Shin splints can be resolved with at-home remedies. Only in the rarest of cases do they need surgery. The main way to avoid shin splints from reoccurring is to make sure you are not pushing past your body’s limits in exercise.
Anatomy
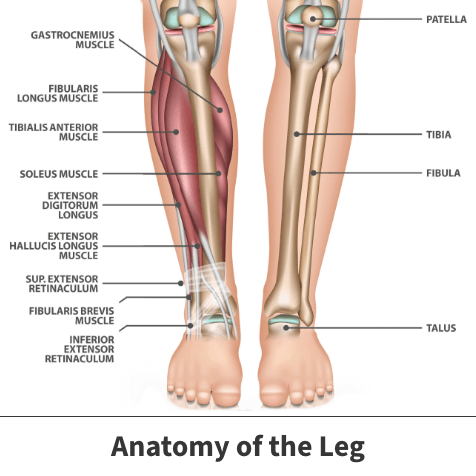
Your legs are made up of several important bones located in your lower leg’s frontal area. One is known as the shinbone (the tibia).
Shin splints are caused by pain along the inner edge of the shinbone. Pain occurs when the muscles, tendons, and bone tissue around the tibia become worn or inflamed due to physical activity or exercise.
The inner border of the tibia where the muscles attach to bone is where pain generally occurs. The tibia/shinbone is on the inner edge part of the leg, while the fibula is on the outer edge part of the leg. Both bones work together with the muscles and other leg parts to provide motion and support.
About
What are shin splints? As its scientific name might suggest, medial tibial stress syndrome occurs when the shinbone or its surrounding soft tissues and muscles become irritated or damaged. Shin splints can develop when the muscle and bone tissue (periosteum) become overworked from intense physical activity. Although not serious, they can hinder your enjoyment of exercise and day-to-day activity if not evaluated.
Causes
Typically, shin splints result from intense, repeated strain on the shin precipitated by some type of forceful movement or athletic activity. Runners, dancers, and military recruits are a few groups who regularly get shin splints.
Shin splints usually happen after unusual or sudden changes in activity – from starting a new workout routine or playing a different sport than you’re used to.
Other factors that contribute to shin splints include:
- Having flat feet
- Exercising in improper or ill-fitting footwear
- Having abnormally rigid arches
If your stance is not corrected, flat feet create stress that can cause shin splints. Changes in intensity or length of exercise also can play a role in adding stress to your shins.
Risk factors
You may stand at greater risk of contracting shin splints provided you engage in an increased amount of exercise or are employed in a job demanding such feats. The injury is commonly seen in:
- Short and long-distance runners
- Walking or running on uneven or steeply-inclined surfaces
- Running or walking on hard surfaces like concrete
- Those undergoing military training
- People who train while wearing the wrong footwear
- Those with flat feet or arches
Shin splints also tend to occur or worsen when you begin a new exercise program or an activity with greater frequency and intensity.

Symptoms
Shin splints can occur before, during, and after exercise. Although not considered a severe injury, shin splints can be painful depending on the intensity of the stress on your shinbone.
The most apparent symptom suggesting the presence of shin splints is pain along the front of your lower leg. In the condition’s earliest stages, this pain may end once you finish exercising. The pain can range from a mild throbbing to a severe, stabbing ache shooting along the border of the tibia. In moderate to severe cases, the associated discomfort could be non-stop and make exercising or performing simple actions challenging.
Besides pain, you might also experience inflammation. While mild swelling can occur, it is less likely if it is only a minor injury. In many instances, inflammation results in swelling, redness, and soreness visible in your lower leg. Pain may be aggravated if the sore spot is touched, as it is likely to be tender.
Complications
If not treated soon after, some shin splints cases might lead to surrounding soft tissue injuries or even stress fractures of the affected bone.
Diagnosis
Usually, shin splints are not difficult for your family doctor or orthopedic specialist to diagnose. Often, this conclusion can be reached after giving your lower leg a complete visual and physical examination.
During a physical examination, your Florida Orthopaedic Institute physician will ask about your symptoms and medical history. Your physician will check for area tenderness and may order imaging tests depending on severity to better see the damage done.
Although shin splints themselves are minor issues, it is important for your physician to carefully examine the area to ensure no other problems are present. Such issues can include:
- Stress fracture – A small crack or cracks in the tibia caused by overuse. Imaging tests such as an X-ray, CT (computerized tomography) scan, or MRI (magnetic resonance imaging) may be ordered to rule out the presence of stress fractures.
- Tendinitis – The inflammation of the tendons that attach muscles to bones. Partial tears of the tendon may cause pain. MRI imaging tests can determine if there are tears present in the tendons.
- Chronic exertional compartment syndrome – A rare condition that mimics the symptoms of shin splints. Caused by built-up pressure within the muscle, chronic exertional compartment syndrome occurs with intense exercise. Although painful, this condition normally subsides after the physical activity has stopped and can be diagnosed through a pressure test.
Your physician will discuss your options with you should they suspect that you have any of these more serious conditions.
Treatment
Most incidents of shin splints can be managed using traditional, non-aggressive treatments. Since they can usually resolve themselves either alone or with at-home remedies, treatment is basic.
Shin splints come about after overuse during intense physical activity, so most standard treatments include some degree of rest to let the injury heal. Your physician may also tell you to take over-the-counter medication to relieve any pain or swelling of the area.
Only the most severe cases need surgery.
Nonsurgical treatments
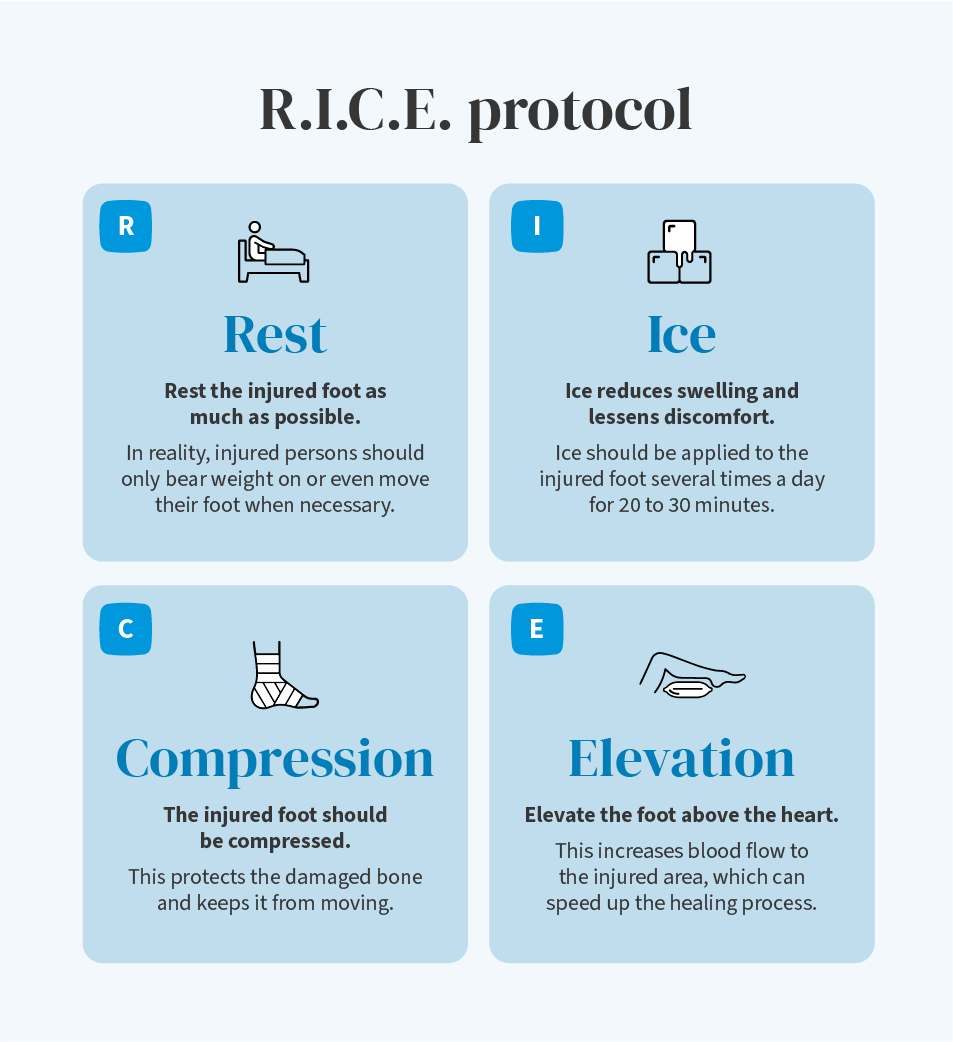
The Florida Orthopaedic Institute’s philosophy is to try all appropriate nonsurgical methods to increase mobility and function first. Shin splints heal naturally if there isn’t any added stress to hinder the healing process. Mild to moderate occurrences usually respond to relatively simple, self-care efforts such as:
- Rest – Staying off or significantly limiting the pressure placed on the affected shin should reduce associated discomfort, inflammation, and soreness. The most critical factor in healing is to avoid high-intensity exercise or sport. Physical activities with little-to-no impact on your feet/legs, such as swimming or a stationary bike, are recommended while recovering from shin splints. Engaging in them will help preserve your leg’s strength and range of motion.
- Ice – You might find relief through the application of ice packs placed over the injured shin. Using cold packs for 20 minutes at a time, multiple times per day can help with swelling. They should be changed and applied frequently, and remember to never apply ice directly to the skin.
- Compression – Your physician may recommend you wear an elastic compression bandage to prevent additional swelling and get you back on your feet quicker. This helps keep the damaged shin in place to prevent further injury.
- Flexibility exercises – Gentle stretching of the lower leg muscles introduced gradually can reduce stress in the shins.
- Over-the-counter medicine – Your doctor may suggest using over-the-counter pain or non-steroidal anti-inflammatory medicines such as ibuprofen (Advil, Motrin) and aspirin for pain reduction.
- Supportive shoes – Your physician may recommend wearing shoes with more cushioning in them to support your shins as they heal. They may also recommend shoe inserts. These extra-cushiony and low-stress inserts can be custom-made to fit your foot or purchased in stores.
- Light physical therapy – Occasionally, therapeutic exercises like stretching keep the surrounding muscles strong and speed up the healing process.
Your Florida Orthopaedic Institute physician will instruct you when it is acceptable to return to exercise. This will be a gradual process, as it is important not to disrupt healing. Before returning to exercise, you should be without pain for at least two weeks. You will also be advised not to return immediately to a regular high-intensity routine or workout.
Warming up and stretching are key to a positive recovery. Shin splints can resolve themselves within a few weeks with proper rest and low-intensity movement. Still, if you feel any pain as you return to exercise, stop immediately and ice the area. Slow training and gradual intensity are essential to avoiding shin splints in the future.
Surgical treatments
Luckily, only the severest cases of shin splints need surgery. Surgery can be done in the rarest of instances, but only if your injury does not respond to nonsurgical treatment.
Surgeons sometimes perform an intervention with small cuts made in the fascia tissues of your surrounding calf muscles. Known as fasciotomy, this surgery is designed to ease pressure on surrounding shin bones and offer relief from shin splint symptoms.
Surgery can be done in the rarest of instances, but that is only if your injury does not respond to nonsurgical treatment.
Your Florida Orthopaedic Institute physician will discuss options with you about any problems that may need surgical attention.
Prognosis
Setting a specific time for the healing process to be completed is difficult. Everyone heals at their own pace, and recovery is often also determined by the condition’s underlying cause and severity. Pain should ease within several weeks. Full healing of the injury could take months.
Several indications have been established that suggest that your shin splints have completely healed, including:
- Your injured leg is as flexible as the non-injured one
- The damaged leg regains the strength of the healthy leg
- You can engage in activities you previously did without any sort of pain
Physicians caution you not to return to full action too quickly. This could delay healing or leave you at an increased risk for developing complications like stress fractures.
Should you receive an official medical diagnosis and follow the treatment program established by your doctor, the injury should heal completely and without any lingering complications.
Prevention
You might lessen your chances of developing shin splints by engaging in efforts including:
- Wearing arch supports
- Wearing the appropriate footwear and replacing running shoes following every 350 to 500 miles worth of distance
- Stopping and resting when experiencing any level of discomfort
- Practicing strength training exercises geared towards strengthening your ankles and lower legs
Above all, the moment you encounter the symptoms of shin splints, visit your doctor as soon as possible to receive a formal diagnosis and treatment plan.
Videos
Related specialties
- ACL Injuries
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Total Knee Replacement Surgery
