Total knee replacement
Surgery for knee replacement
When the pain, discomfort, stiffness and reduced mobility don’t improve with nonsurgical or conservative treatments, an orthopedic physician specializing in knee care may recommend a partial or total knee replacement to help you regain movement and alleviate discomfort.
Developments in surgical practices, coupled with innovative technologies, make the replacement of your entire knee one of the most successful types of orthopedic surgery. In fact, total knee replacement surgeries continue to grow yearly, with almost a million successful replacements each year in the United States alone.
Keep reading for our complete knee replacement FAQ and learn more about:
- What a full knee replacement is,
- Who benefits from this surgical knee repair and
- What to consider when choosing a knee surgeon.

Anatomy
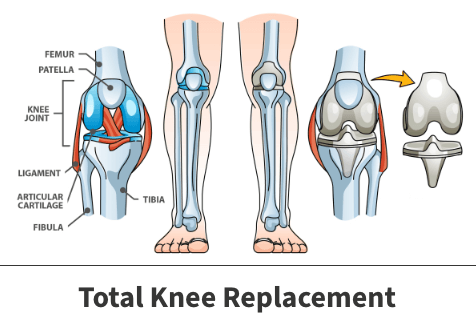
The knee is a hinge joint, meaning it can only bend in one direction. It is where the tibia, the femur, and the patella meet. Like most joints in the body, the knee joint is lined with articular cartilage. The articular cartilage acts as a shock absorber and allows smooth and stable movement. When the articular cartilage wears away, knee replacement can alleviate pain and restore both movement and function.
What is total knee replacement (TKA)?
A total knee arthroplasty (TKA) or knee joint replacement surgery involves replacing the worn-out, diseased knee cartilage with metal and plastic materials designed to restore knee motion and function.
Watch Dr. Michael A. Miranda explain what happens during knee replacement
What happens during the actual surgery for complete knee replacement?
At a high level, a total knee replacement surgery follows these four steps:
- First, you’ll receive anesthesia—either general (putting you to sleep) or regional (numbing the lower half of your body)—so you’re comfortable and don’t feel any pain during the procedure.
- The surgeon starts by making an incision to access your knee joint so they can carefully cut and remove the diseased cartilage and bone from the ends of your femur (thigh bone) and tibia (shin bone). The surgeon then caps the cut bone surfaces with metal implants, effectively restoring the shape and dimensions of the knee joint surfaces. Each of the metal implants on the bone ends then mate with and glides on a special, extremely smooth plastic spacer called polyethylene.
- For many patients, the surgeon will also cut a small portion of the patella and implant a plastic cap.
- Once everything is confirmed to be securely in place and aligned correctly, the surgeon closes the incision and applies a dressing to protect the wound.
The patient is usually moved to a recovery area after surgery. Physical therapy to restore movement and strength starts immediately, and most patients can begin walking with assistance shortly after surgery. They gradually increase their activity levels as they heal.
See how a personal trainer is back to helping others after two knee replacements
What is life like after having new knee replacement surgery?
Recovery from a total knee replacement usually involves several weeks of home physical therapy followed by four to six weeks of outpatient physical therapy, which strengthens the knee and helps restore movement and range of motion.
Most patients start walking with assistance soon after the surgery and gradually increase their activity levels. While recovery times can vary, many individuals can resume their daily activities within six weeks to three months, experiencing improved mobility and reduced pain.
Ongoing exercises and follow-up appointments with your healthcare team are essential to ensure a smooth and successful recovery.
Typical outcomes of full knee replacement
Total knee replacement surgery is often highly successful. According to the American Academy of Orthopaedic Surgeons (AAOS), studies show that approximately 90–95% of knee implants remain functional and pain-free 10 to 15 years after the procedure.
The National Joint Registry’s research findings show that most patients experience significant improvements in mobility and quality of life after surgery, with 85–90% reporting high satisfaction levels.
Discover how knee replacement at FOI helped one biker ride his Harley once more
Potential total knee replacement complications
Complications for patients after total knee replacement are relatively rare, occurring in less than 5% of cases, according to the Centers for Disease Control and Prevention (CDC). Problems may include infections, stiffness, mechanical implant issues and blood clots.

Procedures related to surgery for knee replacement
In addition to the standard total knee replacement, there are several specialized procedures—designed to address specific needs and enhance quality of life—such as:
- Partial knee replacement,
- Bilateral knee replacement and
- Knee revision surgery
Partial knee replacement
Your knee has three compartments: the medial (or inside compartment), lateral (outside compartment), and patellofemoral (front compartment).
A partial knee replacement, or unicompartmental knee arthroplasty (UKA), involves fixing only one of the three compartments (leaving the other healthy compartments and ligaments as is). In contrast, a surgeon replaces all three compartments during a total knee replacement. The parts that need substituting determine whether a knee replacement is partial or total.
A surgeon replaces only one damaged joint compartment in a partial knee replacement, leaving healthy compartments and ligaments intact. This option often leads to a quicker recovery, provides a more natural feeling to the knee, maintains more bone and ligaments and preserves more of your natural mobility.
Learn more about partial knee replacements
Bilateral knee replacement
Bilateral knee replacements involve replacing both knee joints simultaneously. This may be a good choice if you have severe arthritis in both knees and want to undergo only one surgery and recovery process. However, it has downsides, including a higher risk of complications after the surgery. You should discuss this option with your surgeon.
Knee revision surgery
Surgeons may recommend knee revisions for patients when their replacements stop functioning correctly. In this procedure, artificial knee joints are repaired or replaced to help improve mobility and reduce pain.
Hear Dr. Spencer Smith talk about helping patients with failed knee replacements
Surgical approaches for complete knee replacement
Multiple approaches for total knee replacement are available, including the medial parapaterllar as well as midvastus and subvastus approaches. Each offers different benefits.
To ensure a successful surgery and smooth recovery, a knee surgeon will choose the best total knee replacement surgery approach for you. They’ll consider your specific situation, needs and other factors (such as your anatomy, activity level and previous knee problems).
Medial parapatellar approach
Historically considered the standard incision for new knee replacement surgery, the medial parapatellar approach involves accessing the knee joint through the inner (medial) side of the kneecap.
- Benefits: The medial parapatellar approach gives knee surgeons a clearer view of the knee, making it easier to insert a new artificial joint accurately into place.
- When It’s Used: This approach is often chosen for patients who need thorough knee joint cleaning or who have more complex knee issues.
Midvastus and subvastus approaches
The midvastus and subvastus approaches to total knee replacement are minimally invasive because of smaller incisions through the quadriceps (thigh) muscle.
Who benefits from knee arthroplasty?
The knee is a hinge joint, meaning it can only bend in one direction. It’s where the tibia, the femur, and the patella meet. Like most of the body’s joints, the knee is lined with articular cartilage. The articular cartilage acts as a shock absorber, allowing smooth and stable movement. When the articular cartilage wears away, knee replacement can alleviate pain and restore movement and function.
If you have severe knee pain and limited movement due to arthritis or joint damage, knee arthroplasty can help you regain your everyday activities and improve your quality of life.
What is knee arthritis?
Arthritis is an indication that you’ve lost or experienced significant damage to your knee’s cartilage. It’s similar to a tire losing its tread.
The severity of arthritis is often determined based on X-rays and is defined by how thin the knee’s cartilage has become. In cases of “bone-on-bone” arthritis, the disease is very serious.
What are non-invasive treatment options?
Chronic knee arthritis can significantly disrupt daily life, making walking and climbing stairs more difficult. Simple tasks—such as getting in and out of cars or rising from chairs—can become painful and exhausting. Conservative treatment includes physical therapy, non-steroidal anti-inflammatories (NSAIDs), Tylenol, and various injections.
The most common injection performed is a corticosteroid, which is a powerful anti-inflammatory. We also offer specialty injections and other advanced therapies to support tissue health and recovery. The effectiveness of each option varies and should be discussed independently with your surgeon.
How do I know if I need a knee replaced?
Deciding whether to undergo knee replacement is a significant step. Although it’s considered a safer orthopedic procedure, total knee replacement is still a major operation, so it’s natural to question whether it’s right for you.
Here are examples of when it might be time to think about having complete knee replacement surgery:
- You’ve exhausted conservative treatment options without satisfactory relief.
- Your pain and loss of knee function make it hard to perform everyday tasks and enjoy activities you love.
- You’re in good overall health and medically fit for surgery—able to tolerate anesthesia and rehabilitation.
- You’re mentally prepared for total knee replacement surgery and motivated to participate in the post-operative recovery process.
If surgery for knee replacement might be right for you, schedule an appointment to discuss your symptoms, medical history, and treatment options with an experienced knee surgeon.
Find out how a custom knee implant helped a 77-year-old CEO golf again
Advances in surgery for knee replacement
Since the first total knee replacement surgery was performed in 1968, surgery to replace the knee joint completely has continually evolved in its usefulness, effectiveness, and overall success. Recent innovations and improvements in total knee replacement surgery have significantly enhanced patient outcomes and recovery experiences.
Robot-assisted and computer-guided procedures improve the precision of implant placement and alignment, which may impact long-term results and implant survivorship. Additionally, outpatient (or same-day) knee replacement surgeries allow eligible patients to return home the same day, reducing hospital stays and promoting quicker recoveries.
Watch Dr. Thomas L. Bernasek talk about the benefits of outpatient joint surgery
New pain management techniques, including improved anesthesia protocols and targeted pain control strategies, help minimize post-operative discomfort and enable patients to begin physical therapy sooner.
These advancements collectively make knee replacement surgeries safer, more efficient, and more comfortable, allowing patients to regain mobility and quality of life more smoothly.
Hear Dr. Hari Parvataneni share why he considers patient relationships as partnerships
Selecting a surgeon for full knee replacement
Identifying the right surgeon for your knee replacement is a crucial step toward a successful surgery and recovery. Research the providers you’re considering and evaluate the following factors to make an informed decision:
- Experience and expertise: Look for a surgeon specializing in knee arthroplasty and inquire about their success rates. Research suggests that patients who select surgeons with joint replacement surgery fellowship training achieve better outcomes than people who pick surgeons without such specialized qualifications. Additionally, those who have the expertise to manage joint replacements that have failed are often more experienced in managing complex issues that may arise.
- Convenient care options: Make it easy on yourself. Choose a knee replacement surgeon who’s part of a robust orthopedic health system (with various locations and comprehensive services). By doing so, scheduling may be more flexible, and getting coordinated care—for everything from imaging to physical therapy and rehabilitation—might be easier, too.
- Patient feedback: Seek referrals from trusted friends and family members, or ask your primary care provider. You can also gauge others’ surgery for knee replacement experience satisfaction with a provider by researching reviews and reading patient testimonials.
Discover how knee replacement at FOI changed a U.S. Army vet’s life for the better
Why choose FOI for total knee replacement
Complete knee replacement surgery is considered one of the most successful medical operations. At Florida Orthopaedic Institute, our fellowship-trained knee surgeons are renowned specialists in orthopedic care. They combine their world-class training with innovation to provide patients individualized solutions designed to help them stay active.
Picking the right surgeon is essential for a successful knee replacement. Our team is here to support you with expertise, convenience, and comprehensive care. When ready, contact us to schedule a knee replacement consultation at FOI.
During this appointment, you can discuss your options with a surgeon, explore treatment plans, and determine the best surgical approach for your needs.
Listen to an active retiree reveal what life is like after having two knee replacements
Total knee replacement FAQs
The most challenging day after a total knee replacement is often the first day after surgery when you wake up and start feeling immediate discomfort and swelling.
Moving for the first time can be challenging as your body adjusts to its new knee. Pain and stiffness are common, making even small movements feel difficult.
Additionally, for some patients, dealing with emotions and fatigue adds to the overall difficulty of beginning their recovery journey after having surgery for new knees.
Yes! Some patients can undergo outpatient surgery for complete knee replacement using advanced surgical techniques and comprehensive care plans. This approach allows eligible individuals to go home on the same day as their surgery, promoting a quicker recovery and greater comfort.
Watch Dr. Grant G. Garlick talk about outpatient knee replacements at FOI
Following your doctor’s instructions on taking pain medication can help ease pain after a complete knee replacement.
Applying ice packs to your knee can help reduce swelling and numb the area, providing additional relief. Engaging in gentle physical therapy exercises, as recommended, can strengthen your muscles and improve mobility, which also helps manage pain. In addition to these recommendations, experts often advise keeping your leg elevated when resting and avoiding putting excessive strain on the knee, which can further minimize discomfort.
Generally, it’s not recommended to drive two weeks after a total knee replacement. Most doctors advise waiting at least three to six weeks before getting behind the wheel to ensure your knee has healed enough and you have regained sufficient strength and mobility.
Driving too soon can increase the risk of accidents or complications as your reaction time and leg control might still be limited.
Always follow your surgeon’s specific advice based on your recovery progress.
Robot-assisted total knee replacement uses advanced robotic technology to help surgeons precisely plan and place your new knee joint. This extra level of accuracy can lead to a smoother recovery and better overall results.
It’s always best to consult your surgeon or physical therapist if you have questions about what you can or can’t do after surgery. Every patient is different, but kneeling after knee replacement is generally possible.
While doing so shouldn’t harm your artificial knee or shorten its life, kneeling when you have an artificial knee might make you feel unstable. If you do decide to try kneeling after you’ve healed from surgery, take it slowly. Start by kneeling on a padded surface, then gradually build up your time in that position before moving to harder ground.
Be patient with your progress.

Should you see a specialist about your knee pain? Answer these questions to find out.
Videos
Related specialties
- ACL Injuries
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
