Anatomy
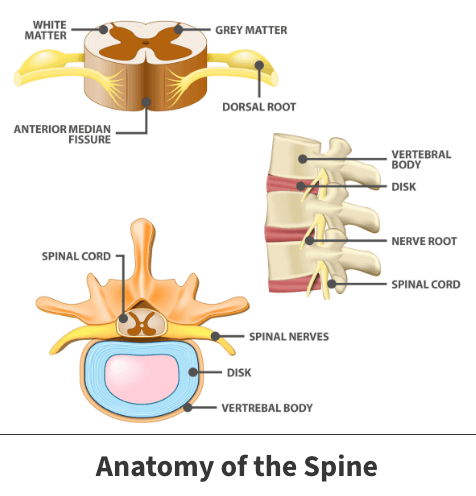
Between the bones (vertebra) of the spine, you have components called discs. Discs are made up of a hard, tough outside and a soft interior. Discs provide a cushion between your spine’s vertebrae. They are necessary to help carry out everyday activities like walking, bending, and twisting.
About
When discs wear down or sustain any type of injury, you can experience degenerative disc disease symptoms. Degenerative disc disease occurs when there are structural changes of the disc’s outer surface and inner sections.
Causes
Disc degeneration can result from several different underlying causes, including age, trauma, and illness. While everyone will experience some degree of disc degeneration as they age, not everyone will feel pain or other symptoms. Acute traumatic events like automobile accidents can result in disc damage. Additionally, various systemic diseases can result in disc decline.
Cracking is another cause of disc degeneration. The spine is the focal point of your body’s physical structure and capabilities. That said, movements like bending, shifting, and twisting performed countless times per day over many years take their toll on spinal discs. Eventually, such strain causes small cracks to occur on your disc’s outer walls. The outer walls contain nerves, which, if pressed upon, can be painful.
Larger cracks can allow the disc’s softer, inner part to escape. If this happens, the disc in question can shift out of place or swell. Such an event is called a herniated or slipped disc. This condition can also impact neighboring nerves, produce discomfort, and cause other associated symptoms.
Cervical discs are made up of mostly water. As you age, a disc’s water content decreases, causing the disc to thin out and flatten. Thin, flattened discs are less capable of withstanding pressure. Less water also equals reduced protection between your vertebrae. This leaves vertebrae and surrounding bones more vulnerable to rapid breakdown and injury.
Symptoms
The symptoms you experience may vary depending on factors such as where in your spine the injured disc is located, the extent of the damage, and the specific cause. You might expect to have one or more of these relatively common symptoms, like:
- Back or neck pain
- Sharp, stabbing pain
- Discomfort that comes and goes (or can be continual)
- Pain that worsens when you perform movements like bending or twisting
- Uncomfortable feeling that might ease when you change positions or lie down
In moderate to severe instances, you may also experience a tingling sensation or numbness in your arms and legs, and muscle weakness in your legs. These more pronounced occurrences typically mean your discs are pressing on spinal nerves.
Diagnosis
Reaching a clear and firm diagnosis can take time, investigation, and examination by your doctor. Spinal disc degeneration can be initially diagnosed by your family physician or an orthopedic specialist by performing a thorough physical assessment.
Should the examining doctor believe that you might have disc degeneration, they will first likely ask you several questions such as:
- When did the pain begin?
- Where in your back or neck do you feel discomfort?
- Does engaging in activity worsen or lessen the pain?
- Have you sustained any recent back injuries?
- Have you been diagnosed with any type of back, spinal, or physical problem before?
- Do you have a family history of any type of back or spinal issues?
Your doctor might then ask you to walk or perform specific movements. During the final evaluation stage, your doctor may order diagnostic tools such as X-rays or MRI scans (magnetic resonance imaging). These tests allow the attending physician to study images of your spine more carefully. Such images reveal any disc deterioration and help confirm the diagnosis.

Treatment
Fortunately, spinal disc deterioration can be treated. The specific option chosen by your doctor will depend on many issues, including your age, fitness level, general biological and physical health, in addition to the underlying cause and the degeneration’s severity. Therapeutic efforts can range from medications to surgical intervention.
Nonsurgical treatments
Minor to moderate cases are often treated using nonsurgical treatments such as:
- Physical therapy – Your doctor may prescribe a course of physical therapy. In that case, you will perform several exercises over a specific time period designed to improve the mobility of and strengthen the muscles near where the damaged disc is located.
- Medications – If your pain is tolerable, you might only need pain relievers and inflammation-reducing drugs, readily available over-the-counter. But if associated discomfort interferes with your ability to go about daily tasks, your doctor might prescribe prescription pain medication. More moderate instances might require steroid injections – known for their ability to reduce swelling and inflammation quickly.
- Surgical intervention – Luckily, medications and physical therapy sufficiently address a large percentage of spinal disc degeneration cases. However, when the pain is severe, surgery may be a preferred option. Your doctor might choose to remove a part or all a defective disc. Occasionally, disc removal is followed by fusion surgery, which involves connecting the adjacent spinal bones.
Videos
Related specialties
- Anterior Cervical Corpectomy & Discectomy
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Pinched Nerve
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
