Discectomy
Without question, your spine is one of the most important parts of your body. It provides the central framework connecting your bones, muscles, and soft tissues that perform basic actions like standing, sitting, walking, and bending.
Your spine is a complex network that has many parts. Among them are discs, which are vital to your spine’s strength and health. Discs act as a cushion to your spinal bones (vertebrae). They also aid in holding those bones in place and enable spinal movement.
Should your spinal discs experience damage or illness, you may find relief through the medical procedure discectomy.
Anatomy
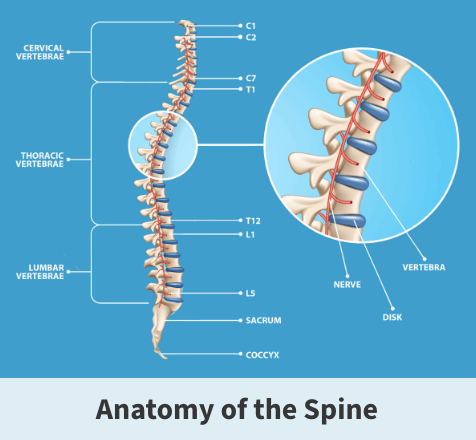
Discs are found throughout the spine, which is divided into three sections:
- Upper – cervical spine
- Center – thoracic region
- Lower – lumbar spine
About
Over time or due to various injuries and illnesses, spinal discs can experience deterioration (herniation). Discs are made up of two parts. The center is soft and filled with a jelly-like substance, while the exterior is a stronger, fiber-like material. Herniation occurs when a disc’s center extends into and damages the outer part.
Causes
There is no one specific cause for disc herniation. It is believed that it results from:
- Age – As you grow older, your spinal discs lose their flexibility. This can leave discs at greater risk of tearing or even completely rupturing.
- Poor posture – Having poor posture for years while walking, sitting, or standing up can weaken the spine and eventually result in disc problems.
- Excessive pressure – Working a job or participating in a sport/recreational activity requiring bending, lifting, or physical contact can place added pressure on spinal discs and eventually lead to herniation.
- Acute trauma – Disc damage can also occur following a traumatic event like a fall or car accident.
Risk factors
Your risk of developing a disc injury increases if you:
- Smoke – Researchers believe that cigarette smoking reduces the amount of oxygen transported to spinal discs and makes them more likely to break down
- Are overweight – If you are overweight or obese, you place a great deal of added pressure on your spinal discs
- Carry a genetic predisposition – Certain genetic flaws can contribute to back deformities, leading to disc damage and eventual herniation
Symptoms
Though most commonly seen in the lower back, herniation could occur anywhere along your spine. The symptoms you experience will depend on the specific location of the injury and the severity.
Symptoms are typically felt on one side of your body and include pain in your arm, leg, foot, buttocks, thigh, or hip. The pain is usually sharp, can radiate to other parts of the body, and is often worsened by various types of movement.
Mild to severe cases may bring numbness in an arm or leg because the damaged discs press on surrounding nerves. You may experience mobility issues as muscles near the affected nerves gradually weaken.
Complications
Herniated discs can lead to serious mobility problems and possibly permanent nerve damage if not detected and treated.
Treatment
Discectomy is beneficial in situations where moderate to severe disc herniation has occurred.
Occasionally, surgeons will only need to remove the part of the damaged disc pressing up against surrounding nerves or other important body parts.
If the deterioration is significant or causes disabling nerve damage, entire discs might need to be removed. This procedure requires a more complex approach by inserting existing or artificial bone. The goal is to fill gaps of open space and fuse together affected vertebrae.
Usually, the operation is performed under general anesthesia, which means you will be asleep until after it is completed.
Preparation
Doctors might ask you to avoid certain foods or limit your intake of specific foods or beverages in the days and hours leading up to the surgery. You need to discuss the medications you are taking with your doctor in case you need to limit them before surgery.
Recovery
If you respond well to surgery and have no other health or physical conditions, you might be able to return home several hours after surgery. You’ll likely need to remain in the hospital for an extra day or two for observation.
Orthopedic surgeons usually recommend waiting six to eight weeks before returning to a physically demanding position. The recovery process will also likely involve several follow-up appointments with your doctor to track the healing process and prevent potential complications. In some cases, patients will undergo physical therapy.
Outlook
A discectomy can usually relieve the nerve pressure and associated symptoms. By addressing the issues that caused the disc damage originally, future problems can help be prevented.
You can reduce your chances of further disc herniation through efforts including:
- Maintaining a healthy weight
- Practicing proper posture
- Exercising
- Wearing back braces or other protective gear if employed in a physically demanding job
Above all, seek medical attention if you experience back pain or other symptoms possibly related to disc herniation. Identifying and addressing the problem as soon as possible can prevent complications or future occurrences.

Videos
Related specialties
- Anterior Cervical Corpectomy & Discectomy
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Degenerative Disc Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discitis Treatment & Information
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Pinched Nerve
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
