Pinched nerve
A pinched nerve is when a nerve in the neck is compressed or irritated where it branches away from the spinal cord. A pinched nerve is often caused by the deterioration of the spine. In most cases, pinched nerves respond well to conservative treatment that includes medication and physical therapy. But if the pinched nerve is severe or does not respond well to non-surgical treatments, there are several surgical procedures available for you. Your Florida Orthopaedic Institute physician will help you figure out which treatment plan or procedure will best help you have a full recovery.
Anatomy
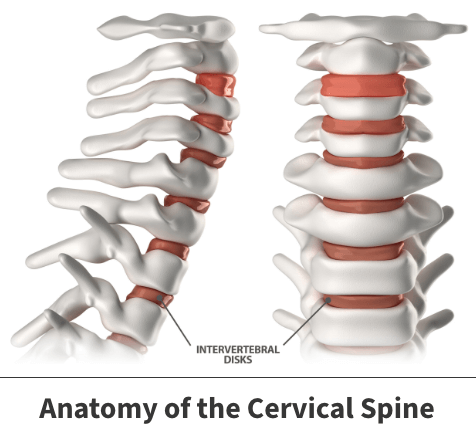
The spine consists of 33 individual bones known as vertebrae that interlock. The vertebrae are categorized into five regions:
- Cervical
- Thoracic
- Lumbar
- Sacrum
- Coccyx
Your spinal cord consists of “electrical cables” that travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through openings in the vertebrae.
Intervertebral discs sit between the vertebrae and are the shock absorbers for the spine. They are flat, round, about half an inch thick and made up of two components—the nucleus pulposus, and the annulus fibrosus. The nucleus has a jelly-like consistency and can be found in the center of the disc. The “jelly” allows the disc to be flexible and strong. The annulus is the flexible outer ring of the disc and consists of several layers. When moving or standing, weight is put on the nucleus, causing it to expand while the annulus holds it in place. Together, the nucleus and annulus allow for movement to take place while simultaneously maintaining the strength of the spine.
About
A pinched nerve, also known as cervical radiculopathy, is when a nerve in the neck is compressed or irritated where it branches away from the spinal cord. A pinched nerve in the neck is often caused by wear and tear changes that occur in the spine as we age. It can also be caused by a sudden injury that results in a herniated disc. As the discs in the spine age, they lose their flexibility and stability, and lose water content, causing them to dry out and become stiffer. As the discs start to grow weaker, your body will begin forming more bone, known as bone spurs, around the discs to strengthen them. These bone spurs cause the spine to stiffen as well as narrow the small openings on each side of the spinal column, the foramen, where the nerve roots exit, pinching the nerve root.
In the case of a herniated disc, the jelly-like center of the disc pushes against its outer ring, causing it to bulge out. When it bulges out toward the spinal canal, it puts pressure on the nerve root, causing pain and weakness in the area the nerve supplies.
Symptoms
In most cases, pain will begin in the neck and travel down the arm in the area served by the damaged nerve.
Certain neck movements, like extending, straining, or turning the neck, may increase pain. Other symptoms may include:
- Tingling in the fingers or hand
- Weakness in the arm, shoulder or hand muscles
- Loss of sensation

Diagnosis
Your Florida Orthopaedic Institute physician will take a look at your symptoms and general health. They will be looking for muscle weakness, loss of sensation, or a change in your reflexes. Your physician may also order some tests to get a better look at your nerves and spine. These tests may include:
- X-rays – This test provides images of dense structures, like bone. It will show the alignment of the bones along your neck and can also show if there is any narrowing of the spinal canal and damage to the discs.
- MRI (magnetic resonance imaging) scans – These tests create better images of the body’s soft tissues. An MRI of the neck can show if your nerve compression is caused by damage to soft tissues—such as a bulging or herniated disc. It can also help your physician determine whether there is any damage to your spinal cord or nerve roots.
- CT (computed tomography) CT scans – This test can help determine whether or not you have developed bone spurs near the small openings on each side of the spinal column.
- EMG (electromyography) – An EMG measures the electrical impulses of the muscles at rest and during contractions. Nerve conduction studies are often done along with EMG to determine if a nerve is functioning normally. Together, these tests can help your physician determine whether your symptoms are caused by pressure on spinal nerve roots and nerve damage.
Treatment
Nonsurgical treatments are the initial treatment plan for pinched nerves. Majority of patients who experience a pinched nerve get better over time and do not need surgery. For some patients, the pain goes away relatively quickly, usually in a few days or weeks. For others, it may take longer. Your physician may recommend surgical treatments only if you do not respond to nonsurgical treatments.
Nonsurgical treatments
The nonsurgical treatment options available for treating pinched nerves include:
- Soft cervical collar – This is a padded ring that wraps around the neck and is held in place with Velcro. It allows for your neck muscles to rest as well as limiting neck movement, which can help decrease the pinching of the nerve roots.
- Medications – Pain relief medications such as aspirin and ibuprofen (Advil, Motrin) may provide relief for the pain that is caused by the pinched nerve. Additionally, a short course of oral corticosteroids may help relieve pain by reducing swelling and inflammation around the nerve.
- Physical therapy – There are specific exercises to help ease pain, improve range of motion, and strengthen neck muscles. In some cases, traction can be used to stretch the joints and muscles of the neck gently.
- Steroid injection – Steroids can be injected near the affected nerve to reduce inflammation. Although steroid injections do not relieve the pressure on the nerve caused by a narrow foramen or by a bulging or herniated disc, they can lessen the swelling and ease the pain long enough to allow the nerve to recover.
- Narcotics – Narcotics medications are reserved for patients with severe pain that is not relieved by other options. They are usually only prescribed for a limited time.
Surgical treatments
If your symptoms do not improve after nonsurgical treatments, your physician may recommend surgical treatment.
- Anterior cervical discectomy and fusion (ACDF) – This procedure involves removing the problematic disc or bone spurs and then stabilizing the spine through spinal fusion. Spinal fusion is when the vertebrae are joined together so that they heal into a single, solid bone.
- Artificial disc replacement (ADR) – This procedure involves removing the injured disc and replacing it with artificial parts, like in hip or knee replacement. The goal of this procedure is to allow the spinal segment to keep some flexibility and maintain a more normal motion.
- Posterior cervical plaminoforaminotomy – During this procedure, the lamina, the bony arch that forms the backside of the spinal canal, is thinned down, which allows the doctor better access to the damaged nerve. He or she then removes the bone, bone spurs, and tissues that are compressing the nerve root. If your compression is due to a herniated disc, your doctor will remove the part of the disc that is compressing the nerve, as well.
Videos
Related specialties
- Anterior Cervical Corpectomy & Discectomy
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Degenerative Disc Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
